What is cervical cancer?
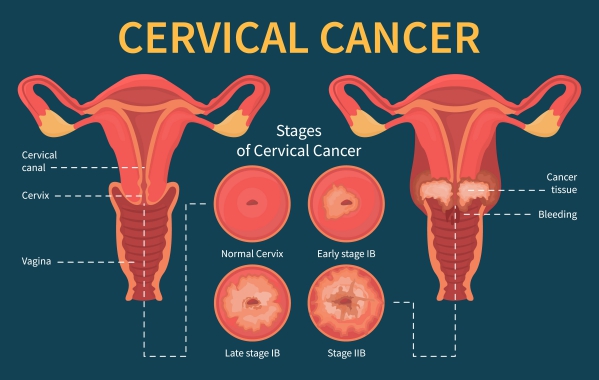
The cervix is a body part present only in females which is the lower end of the uterus connected to the vagina. When cancer arises in your cervix, this is known as cervical cancer. It is the 3rd most common cancer affecting women worldwide. However, it is relatively uncommon in the United States. This may be due to the increase in screening which allows early detection and treatment of the cancer.
It is known to be caused by a virus called the human papillomavirus (HPV). It is common in women who are sexually active. However, most of them usually clear on their own while some may progress to cervical cancer.
The treatment for cervical cancer depends on the severity and degree of involvement of the cancer. In cases where the cancer has invaded surrounding structures, surgery is the required treatment option. In other cases, other therapies may be added on to ensure better management.
Causes of cervical cancer
Human papillomavirus (HPV) must be present for the development of cervical cancer. It is usually acquired during sexual intercourse and is for that reason common among women who are sexually active. While most (90%) usually resolve on their own, some particular cases can evolve into cervical cancer.
The following factors can contribute into the progression to cervical cancer:
 Type and duration of the HPV infection
Type and duration of the HPV infection- Low immune system of host (immunocompromised)
- Coexisting Human immunodeficiency virus (HIV) infection
- Malnutrition
- Smoking
- Vitamin deficiencies
- Lack of screening for cervical cancer
- Early age of first sexual intercourse
- High number of sexual partners
HPV acts as a carcinogen, meaning that it contributes in the development of cancer. It is most commonly transmitted through sexual intercourse, however, some rare exceptions include nonsexual routes of transmission. HPV infection increases your risk of having cervical cancer by 5.
Risk factors for cervical cancer
The following risk factors have been identified for cervical cancer:
- First sexual intercourse at young age
- Having multiple sexual partners
- Having a history of sexually transmitted infections
- Having a promiscuous male partner
Signs and symptoms for cervical cancer
Usually, early stages of cervical cancer do not manifest symptoms. Due to the increase in screening measures and testing for cervical cancer, the only finding at this stage may be an abnormal screening test.
Some of the symptoms that may later start to manifest include:
- Abnormal vaginal bleeding
- Vaginal bleeding after having sex
- Discomfort in vagina
- Malodorous vaginal discharge
- Painful urination
Later stages, where the cancer starts to invade surrounding structures, can manifest with the following symptoms:

- Constipation
- Blood in urine
- Obstruction of the ureters which are tubes connecting your kidneys to your bladder, draining out urine
- Enlarged kidney
- Spread of cancer to lymph nodes, liver, lung or bones
Making a diagnosis
Your doctor will start by asking you a series of questions followed by a physical examination. In early stages, there may be no findings during the physical examination. During later stages, your cervix may appear abnormal upon examination. It may appear as eroded, an ulcer or a mass. If the tumour has eroded the vaginal wall to reach your colon, a rectal examination may reveal the presence of blood.
Your doctor may perform a Papanicolaou (Pap) test to confirm the diagnosis. This test is also used for the screening of cervical cancer in asymptomatic women. In this test, your doctor will insert a small brush through your vagina to scrape some cells from your cervix for further examination in a laboratory, where abnormal cells will be looked for. If the Pap test comes back as abnormal, further testing may be required. A special instrument called the colposcope is used to visualise in more detail your cervix. During this examination, known as colposcopy, samples of your cervix may be taken for analysis. This is called a biopsy. This is performed with the help of a sharp instrument which cuts off small samples of your cervix.

Other tests may also be required throughout the evaluation including
- Cone biopsy: This is procedure whereby deeper layer of your cervix can be obtained for evaluation. This usually requires anaesthesia.
- Complete blood count and serum chemistries: These tests are used to look for any abnormalities in the kidney and liver function as the cancer may spread to these organs.
- Computed tomography (CT) scan or magnetic resonance imaging (MRI): These imaging tests may be required if spread of the cancer is suspected.
Treatment of cervical cancer
Cervical cancer is a treatable cancer and the chances of cure is even higher during early diagnosis. Various treatment options exist with regards to cervical cancer. Your doctor will know best which treatment suits you best depending on the stage of the cancer, your age and general health.
Treatment options for cervical cancer include the following:
- Radical hysterectomy: Radical hysterectomy is the removal of your uterus, cervix, part of your vagina and some surrounding structures. Your ovaries may be left intact depending on cases. Sometimes, during the procedure, lymph nodes found in your pelvis and abdomen may have to be removed for further evaluation. There are different approaches to perform the surgery including laparotomy (through an incision in the abdomen) or laparoscopy (though several small incisions in your abdomen). Studies have shown that laparotomy is associated with better outcomes. The surgery may take a few hours and you will be required to stay at the hospital for a few days. Depending on the case, chemotherapy or radiation therapy may be administered in addition to the surgery.
- Radiation therapy: In this treatment modality, high energy beams are used to kill cancer cells. It can be used in combination with chemotherapy as the first treatment choice for cervical cancer. It can also be used after surgery to decrease the risk of cancer recurrence. Brachytherapy is when the radiation is delivered through a device placed in your vagina and uterus. On the other hand, external beam radiation therapy is when the energy beam is delivered on the outside of your body. Side effects of this treatment may include disturbed bowel and bladder function and narrowing of your vagina. If you are still menstruating, radiotherapy can induce menopause.
- Chemotherapy: Sometimes, chemotherapy is administered together with radiation therapy. This involves injecting anti-cancer drugs through your veins. They work by stopping or slowing the growth of cancer cells. It can also increase the efficiency of radiation therapy.

Complications of cervical cancer
Some of the complications of cervical cancer include the following:
- Invasion to adjacent structures such as the bladder or colon
- Pain if it spreads to bones
- Early menopause
- Inability to get pregnant after removal of uterus
- Narrowing of your vagina leading to painful sexual intercourse
- Bleeding
- Kidney failure due to obstruction to urine outflow
Prevention
The following measures can be taken to prevent the appearance of cervical cancer:

- Get vaccinated: Being vaccinated against HPV can help in preventing the development of the cancer.
- Have routine testing: It is recommended to be screened for HPV through Pap tests on a regular basis especially if you are at high risk of getting the infection. It is recommended to start at around 21 years of age.
- Safe sex: Use appropriate protection when having sex and limit your number of sexual partners.
- Quit smoking: Stop smoking if you do. Do not start if you are a non-smoker.
Prognosis
The course of the disease varies from person to person. There is a high chance of cure if the cancer is detected early. Following treatment, early stages of cervical cancer have an excellent survival rate. If the cancer has spread to lymph nodes, it chance of recurrence after treatment is high.

Source:
J. Alastair, I. and Simon, M., 2016. Davidsons Essentials of Medicine. 2nd ed. London: ELSEVIER.
Boardman, C., 2019. Cervical Cancer.
Straughn, J., 2020. Management of early-stage cervical cancer.