What is COPD?
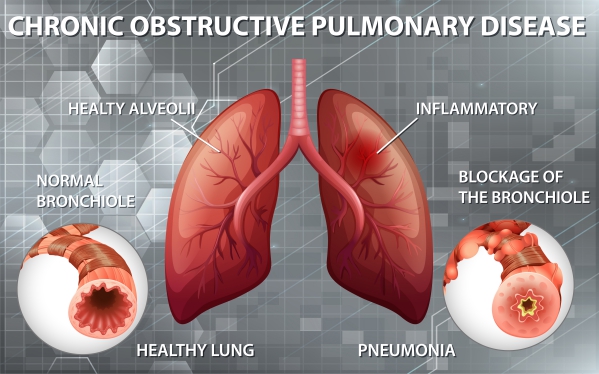
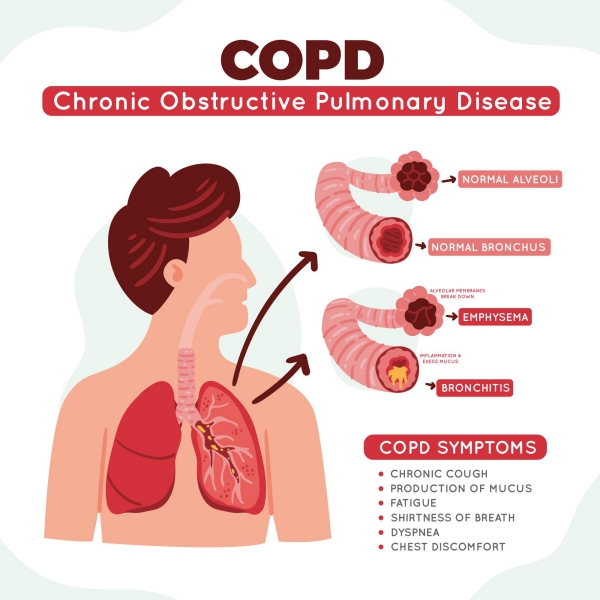
Chronic obstructive pulmonary disease, or COPD, is a term used to group some lung disorders that result in inflammation and obstruction of the airways found in your lungs. This will then result in difficulty in breathing. The two most common disorders are chronic bronchitis and emphysema. Despite being two different conditions, they can both occur simultaneously.
Emphysema occurs when the wall of your air sacs (alveoli) found at the end of your airways are damaged resulting in the merging of different air sacs into a giant one. This impairs absorption of oxygen and you will end up with little oxygen in your circulating blood. On the other hand chronic bronchitis involves the inflammation and narrowing of your airways in addition to the loss of hair like structures (cilia) in your windpipes. The function of cilia is to sweep up the accumulation of mucus and clear out the airways. Eventually, the loss of this important structure will result in mucus build up and chronic cough in an attempt to remove the obstructing mucus plug.
Despite being a chronic condition, and having no cure up to date, treatments are available to reduce the symptoms and decrease the probability of developing complications.
What are the causes of COPD?
The most common cause of COPD is the exposure to irritants such as tobacco smoking. A long exposure to chemical irritants can also lead to COPD. These irritants include exposure to fumes from burning fuel and or some other kinds of air pollution for a long duration.

Passive tobacco smoking, which is standing next to a person who is smoking and inhaling the second-hand smoke, can also increase your risk of having the condition. If you are a known case of COPD and are still smoking, your condition will deteriorate faster.
It is also important to note that COPD is not a contagious disease.
Who are at risk of having COPD?
You are at increased risk of having COPD is you have asthma and smoke concomitantly. In some rare cases, some patients may be having a genetic disorder called Alpha-1-antitrypsin deficiency. Alpha-1-antitrypsin is an important protein which protects your lungs. You can also be at increased risk if you are exposed to inhaled irritants at your workplace.
Signs and Symptoms of COPD
The combination of the inflamed airways and the impaired clearing of mucus results in a variety of symptoms. Initially the symptoms may not be very apparent but as the disease progresses, they become more present and impairing.
The initial symptoms include:
- Occasionally feeling out of breath mostly after physical activities
- Recurrent coughing
- The need to often clear your throat mostly as soon as you wake up in the morning
Later, the evolution of the symptoms may be as follows:
- Difficulty in breathing, which gets worse during physical activities, or during even mild activity
- Chronic cough which does not go away with or without mucus
- Squeaking sound in your chest when you breathe
- Tight feeling in the chest
- Lack of energy
- Frequently having colds or flu (recurrent infections)
- Swelling in your lower extremities
- Unexplained weight loss

More severe presentations include:
- Having blue fingernails or lips resulting from very low levels of oxygen in your circulating blood
- Having difficulty to breathe even while talking
- Feelings of confusion or about to faint
- Feeling that your heart is beating really fast
If you notice any of the above symptoms, you are advised to seek medical help as soon as possible.
Making a diagnosis
To come up with a diagnosis, your doctor will first start by taking a detailed history, focusing on your exposure to irritants, and performing a physical examination. You will then be required to undergo certain tests to further confirm the diagnosis of COPD. It is important for you to explain clearly what your symptoms are and the progression of the condition.
Your doctor will examine your respiratory system with a stethoscope to listen for any abnormal sounds. Some further tests may include:
- Chest X-ray or CT scan: These tests will enable detailed visualisation of your lungs and other important structures. They are also helpful to rule out other conditions that can give you similar symptoms.
- Spirometry: This is also known as lung function tests. It is used to calculate the amount of air that you are able to inhale and exhale. It also indicates how well your lungs are functioning with respect to oxygen delivery. The test is performed by blowing into a tube connected to a small monitor.
- Arterial blood gas: This is a more accurate test to show how well your lungs is distributing oxygen in your body.

Treatment of COPD
After taking a proper history and examination, your doctor will use all the information to stage the severity of your disease according to the GOLD criteria. This staging will guide in choosing the most appropriate treatment for you. There is no cure for COPD. However, proper medications can ease your symptoms and prevent the onset of complications.
Stop smoking
The first and most important step in the management of COPD is to quit smoking. Smoking will make your condition worse and deteriorate a lot faster. Your doctor will advise you on smoking cessation techniques to help you stop smoking using nicotine replacement products and medications. It is also important to prevent exposure to second-hand smoke as this still has deleterious effects.
Medications
There are several drugs that can be used to manage COPD. The use of each of the following depends on the severity of your condition. Your doctor will clearly explain to you when and how to use the medications properly. These medications include the following:

- Bronchodilators: these are medications used in the form of inhalers or nebulizers. They work by widening your airways, which were narrow, in order to make breathing easier and easing your cough. They come in two different form: short-acting and long-acting bronchodilators. The short-acting bronchodilators are mainly used only when you need them, that is, when you feel short of breathe. Their effect last for about four to six hours.
On the other hand, long-acting bronchodilators are intended for everyday use and their effect last for around 12 hours. These medications can also help you to clear away mucus from your lungs. Some inhalers contain glucocorticosteroids which work by reducing inflammation in your airways for example fluticasone and budesonide.
Some examples of short-acting bronchodilators include: albuterol, ipratropium and levalbuterol. Examples of long-acting bronchodilators include: formoterol, indacaterol, salmeterol and tiotropium.
Inhalers with combined bronchodilators and inhaled steroids are also available.
You may experience some side effects following the use of bronchodilators such as constipation, muscular cramps, headache or dry mouth.
- Oral steroids: these are usually used in periods where COPD flare-up (exacerbations). They are given as short courses as the long term use of this drug is not recommended due to the several side effects such as osteoporosis, gain in weight, diabetes, visual problems and an increased predisposition to infections.
- Phosphodiesterase-4 inhibitor: it is a medication mainly used in severe COPD and in patients with symptoms with chronic bronchitis. It acts by reducing inflammation and widening airways. The approved drug found in this group is roflumilast.
- Theophylline: this is a medication used to relieve tightness of chest and prevent exacerbations. However, this is not a drug that doctors usually prescribe as your first treatment.
- Antibiotics, antivirals and vaccines: since your lung is not functioning at its full capacity, you are more prone to respiratory infections. Depending on your condition, your doctor may prescribe you some antibiotics or antivirals to treat your infections. It is also recommended that you get your yearly flu shot, pneumococcal vaccine or the whooping cough vaccine.

Oxygen therapy
Sometimes, the exacerbations are so severe that your levels of oxygen in your body will decrease to abnormally low levels. This will require oxygen therapy whereby you are provided with oxygen via a face mask or nasal cannula.
Surgery
These are indicated in patients with severe forms of emphysema in whom medications are ineffective. These options include:
- Lung volume reduction surgery: in this procedure, a small section of damaged lung tissue is removed. This gives room for the healthy lung to expand properly.
- Lung transplant: you are required to meet specific criteria to be eligible for this surgery. This can improve your capacity to breathe and move around. However, it is a very risky procedure.
- Bullectomy: when the wall of the alveoli are destroyed, they form large air spaces called bullae. In this procedure, these bullae are removed to enable adequate air flow in the lungs.

Managing an exacerbation of COPD
It is of upmost importance to be able to recognise an exacerbation when you have one. These flare-ups can be so bad that you end up staying at the hospital. Some signs that may be indicating a flare-up include lack of energy, onset of fever, signs of a cold, coughing up mucus more than you used to, swelling in your lower extremities and confusion.
Your doctor should explain to you what to do in cases of flare-ups. You should also be able to judge the severity of your exacerbations. For example:
- Mild: if you are getting more breathless but are not coughing more than usual. In that case, using your inhaler may be enough.
- Moderate: if the inhaler in ineffective and you notice that you are coughing more than usual, call your doctor.
- Severe: despite all the medications, your condition is deteriorating or you start having a fever. This requires immediate medical attention. If you cannot reach your doctor immediately, call the emergency services.
Some triggering factors for an exacerbation include smoke or air pollution, cigarette smoke, cold or humid air and pollen.
Complications of COPD
The following summarises the possible complications that can arise from COPD:
- Lung infections
- Poor gas exchange
- Heart problems
- Osteoporosis
- Weak arms and legs
- Sleep problems
- Depression and anxiety
- Lung cancer

Prevention of COPD
The following measures can be implemented in order to avoid developing COPD:
- Avoid smoking and passive smoking
- Use of protective face masks if you are exposed to airborne irritants at your workplace or if you live in an environment with air pollution
- Avoid burning of fuel in a poorly ventilated area
Prognosis of COPD
COPD is a disease that progresses slowly. Most people become aware that they have the condition when it reaches late stages. Once you become a known case of COPD, you will be required to regularly visit your doctor. Proper education about the condition along with clear explanations will help you learn how to deal with the disease to live an almost normal life. The impact of the disease on your life expectancy relies on many factors such as your smoking status or your adherence to the treatment. Your doctor’s role is to evaluate your condition and give you appropriate advice and an idea about what to expect.
Source:
Mosenifar, Z., 2020. Chronic Obstructive Pulmonary Disease (COPD)