What is coeliac disease?
Coeliac disease, also known as gluten-sensitive enteropathy or coeliac sprue, is a medical condition in which gluten (or other related proteins) found in food you consume triggers an inflammatory reaction by your immune system. This inflammatory reaction takes place in your small intestine. Gluten is a protein present in wheat, barley, rye and many other food preparations. Whenever gluten comes in contact with the intestines of a genetically predisposed person, the immune reaction occurs.
With time, repeated inflammatory reactions occurring in your intestines can result in damage to the lining of your bowels. This further leads to impaired absorption of important nutrients in your gastrointestinal tract and this is known as malabsorption. Coeliac disease can arise in people of any age and can affect both men and women. Around the world, about 1% of the total population has coeliac disease. About 1 in 3000 people have the condition in the United States.
Despite having no specific sure, avoidance of gluten can stop the damage caused to your intestines as well as malabsorption.
What are the causes and risk factors of coeliac disease?
The exact cause of coeliac disease is unknown. However, a combination of environmental and genetic factors have been shown to play a role. You are also at increased risk of having the disease if you have:
- A close family member with the same medical condition or dermatitis herpitiformis
- Genetic disorders such as Down or Turner syndrome
- Autoimmune thyroid disease
- Type 1 diabetes mellitus
- Addison’s disease

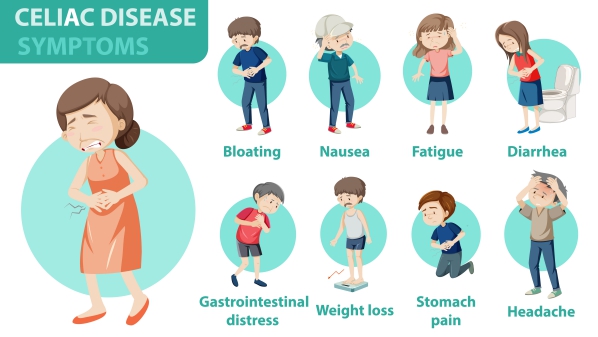
What are the symptoms of coeliac disease?
The symptoms of coeliac disease depend from person to person. There may even be no symptoms at all in people with the mildest form of the medical condition. In other people, the following symptoms may occur:
- Diarrhoea in about 45-85% of all patients, being the most common symptom in untreated coeliac disease
- Foul-smelling, oily, or pale stools
- Dehydration if diarrhoea is severe
- Increased bloating and gas
- Loss of weight
- Weakness and fatigue
- Abdominal pain
- Anemia due to impaired absorption of iron and folate in the small intestines
- Increases bleeding tendency
- Osteoporosis due to decreased calcium and magnesium absorption
- Skin lesions known as dermatitis herpitiformis
- Menstrual disorders such as delayed onset of menses or absence of menses
In children the symptoms include mainly nausea, vomiting, diarrhoea, bloating, increased gas or pale stools. They may also have delayed growth, weight loss, tooth damage and delayed puberty due to malabsorption.
How is the diagnosis of coeliac disease made?

Your doctor will first start by asking you questions about the symptoms you may be having as well as assessing your risk of having coeliac disease. This is done by asking you questions about your general medical status and family history. Your doctor may then request some tests to confirm the diagnosis. These tests are ideally performed while being on a gluten-containing diet. These tests include:
- Serologic tests: These tests are done to identify the presence of antibodies in your blood. This can indicate the presence of immune reactions to gluten.
- Small intestine biopsy: The only way to confirm the diagnosis of coeliac disease after a positive serologic test is to take a sample of your small intestines for further analysis under a microscope. This procedure is called a biopsy. The sample is collected during a procedure known as an upper endoscopy. In this procedure, you will have to swallow a small flexible instrument with a camera on its end. This allows detailed visualisation of the upper gastrointestinal tract and removal of a sample using special instruments. This is not a painful procedure.
- Testing for malabsorption: It is important for you to be tested for any potential deficiencies arising from malabsorption. This includes measurement of iron, folic acid, vitamin B12 and vitamin D levels.
- Other tests: Other tests that can be done in coeliac disease include a complete blood count, lipid levels and thyroid hormone levels. Bone density scans can also be requested to rule out osteoporosis.

How is coeliac disease managed?
The main step in the management of coeliac disease is to eliminate gluten from your diet. Gluten is found in wheat, rye and barley. However, it can also be present in a variety of prepared foods, medications and supplements. Avoidance of gluten requires a lot of lifestyle adjustments.
You may get help from a specialised coeliac dietician who can teach you what foods to avoid and how to replace foods in order to maintain a balanced diet. With time, more and more gluten-free foods are being produced and are available in food stores and supermarkets.
It is recommended that you avoid foods containing wheat, rye, barley, malt, oats and yeast extract. It is also advised to choose foods with gluten-free labels as some foods may be contaminated with gluten.
If you suffer from any deficiencies, your doctor will recommend you taking appropriate supplements.
In some cases, corticosteroid medications may be requires to control the inflammation present in your intestines. They can be used in the presence of severe signs and symptoms of coeliac disease. If you have coexisting dermatitis herpitiformis, a medication known as dapsone may be prescribed.
What are the complications of coeliac disease?
Since there is damage to the lining of your small intestines, coeliac disease can result in malabsorption of essential nutrients and components required by your body. This results in malnutrition, weakening of bones, reproductive problems and problems in your nervous system. It also increases the risk of having cancers such as cancer of the oropharynx, esophagus, pancreas, small and large intestine as well as the liver and biliary system. People with coeliac disease are also at increased risk of having lymphoma which is a cancer of specific cells in your immune system.

Prognosis for coeliac disease
Once the diagnosis of coeliac disease is made and appropriate treatment has been initiated, the prognosis of coeliac disease is excellent. On the other hand, people who are not responding well to gluten withdrawal and corticosteroid treatment have a poor prognosis. Despite rarely causing death, it is a disease that can cause significant impairment and malabsorption, affecting other organs. People with the disease are also at increased risk of having other diseases and complications such as lymphoma and cancer of the gastrointestinal tract.

Source:
Schuppan, D., n.d. Epidemiology, Pathogenesis, And Clinical Manifestations Of Celiac Disease In Adults.
Kelly. C., n.d. Diagnosis Of Celiac Disease In Adults
Ciclitira, P., 2020. Management Of Celiac Disease In Adults.
Goebel, S., 2019. Celiac Disease (Sprue) Clinical Presentation: History, Physical Examination.





