What is colorectal cancer?
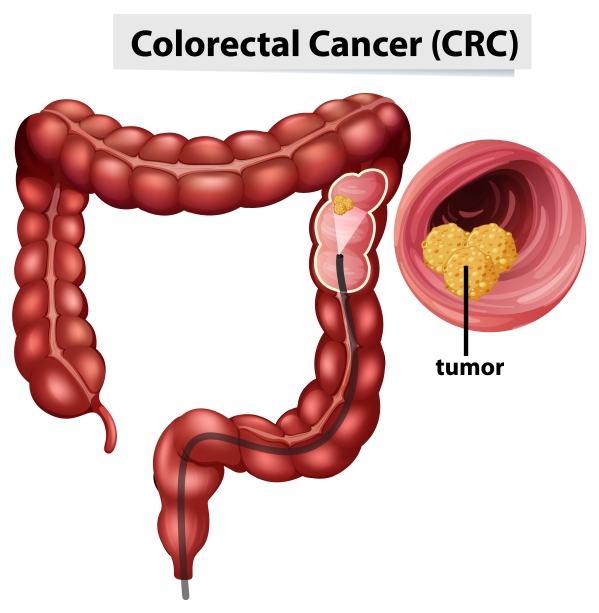
Colorectal cancer (CRC) is a cancer affecting your large intestine and rectum which makes up the final part of your digestive tract. It usually starts as a polyp (an abnormal tissue growth which can be flat or tiny mushroom-like stalks) which then transforms into cancer.
CRC is the second leading cause of cancer death in western countries. In the United Kingdom alone there is about 30,000 cases per year. The American Cancer Society estimates that around 100,000 new cases of CRC will be diagnosed in the United States in 2020.
CRC can be caused by genetic mutation which can be either inherited or acquired. Some symptoms include rectal bleeding, constipation and abdominal pain. Since CRC is a preventable disease, there are screening programs to help identify those at risk of developing it. Once diagnosed with CRC, there are several treatment options such as chemotherapy, immunotherapy and surgical procedures.
Risk factors for colorectal cancer
The risk factors for CRC can be categorised into dietary, lifestyle, medical conditions and genetic factors:
- Dietary factors: increased consumption of red meat, saturated animal fat and alcohol is associated with an increased risk of developing CRC.
- Lifestyle factors: cigarette smoking and sedentary lifestyle increase your risk of developing CRC.
- Genetic factors:

- Familial adenomatous polyposis (FAP): FAP accounts for less than 1% of CRCs whereby numerous colonic tumours appear during childhood.
- MUTYH- associated polyposis (MAP): MAP accounts for a substantial fraction of familial CRCs. Typically, MAP is associated with milder signs and symptoms of colorectal cancer.
- Lynch syndrome (Hereditary Non-Polyposis Colorectal Cancer (HNPCC)): it is the most common form of hereditary CRC. It is characterised by early age of onset and it is present on the right side most frequently.
- Medical conditions: the following medical conditions have been found to be associated with an increased risk of developing CRC:
- Colorectal tumour or polyps
- Ulcerative colitis and Crohn’s disease (inflammatory diseases of the colon)
- Pelvic radiotherapy
- Diabetes
- Cystic fibrosis
- Other factors:
- Advanced age: CRC is most common in people aged greater than 50 years
- African American: People from African American origin are more likely to have CRC.
- Male gender: Men are more prone compared to women
Signs and symptoms of colorectal cancer
There are usually no symptoms in people with early stage colon cancer and they are diagnosed as a result of routine screening. Symptoms of CRC arises due to the growth of the tumour in the intestine. The signs and symptoms of CRC include:

- Change in bowel habits- diarrhoea and constipation
- Rectal bleeding
- Abdominal pain
- Abdominal mass
- Tenesmus (cramping rectal pain): this is a feeling that you need to have a bowel movement even if you just had one. It usually results in only a small amount of stool during the bowel movement.
- Anaemia
- Change in stool colour and shape (narrowed stool)
Late stage symptoms may include unintentional weight loss, excessive fatigue and weakness. In addition, if the cancer is spreading to adjacent structures, you may have symptoms like jaundice, breathing difficulty, severe headaches and puffy hands & feet.
Making a diagnosis
To make a diagnosis, your doctor will first take a history to know more about your symptoms. This is usually followed by a physical examination whereby your doctor will look for signs of CRC. If your doctor suspects a CRC that is located at the end of your digestive tract, he/she will carry out a digital rectal examination (DRE). This involves your doctor inserting a finger into your rectum to assess for any mass or blood.
Your doctor may order a faecal occult blood test to assess whether there is blood in your faeces. This test is usually positive in CRC. In addition, he/she may order additional tests such as complete blood count, serum chemistries, liver function test, renal function test and serum carcinoembryonic antigen (CEA) level. When the CEA level is elevated, it indicates an advanced stage of CRC.

Colonoscopy is an imaging technique that involves passing a tube that has a camera attached to its end into your large intestine. It is usually the investigation of choice for CRC as it allows your doctor to have a direct visualisation inside your large intestine. In addition, if any mass is identified, your doctor may take some samples to be analysed in the laboratory for confirmation of the diagnosis. If a polyp is identified, it can be resected during the colonoscopy procedure. Furthermore, the American College of Gastroenterology recommends colonoscopy every 10 years, beginning at the age of 50 years, as a screening strategy. A flexible sigmoidoscopy can be performed if any mass is felt during the DRE.
Treatment of colorectal cancer
The treatment of CRC usually involves a surgical procedure. However, prior to the procedure, a computed tomography (CT) scan of the abdomen and chest is performed to assess the spread and exact location of the mass. Surgery aims to cure and increase survival time by up to 50%. Nowadays, a laparoscopic surgery can be performed whereby your doctor removes the mass without having to make an incision on your abdomen.
If the mass is located near your caecum, ascending or transverse colon, a right hemicolectomy is done. In this procedure, the right half of your large intestine is removed. On the other hand, if the mass is located in your descending colon or rectum, a left hemicolectomy is done whereby the left half of your large intestine is removed. If the mass is present near your rectum (<8cm from the anus), a permanent colostomy is done following the removal of the mass. This means that the cut end of your intestine is connected to the outside of your abdomen so that your faeces can be collected into a special bag called the colostomy bag.

Radiotherapy is usually performed prior to the surgical procedure but can also be done after if there is any risk of recurrence. Chemotherapy is mainly used in people who have advanced CRC or metastatic CRC (spreading of the cancer).
Complications of colorectal cancer
If CRC is left untreated, it can cause serious complications such as:
- Haemorrhage
- Intestinal obstruction- the mass occludes the large intestine completely which results in faecal retention, leading to intestinal perforation.
- Intestinal perforation- due to the increase pressure building up from the accumulation of faeces inside the large intestine.
Prevention of colon cancer
A large number of factors can contribute in decreasing your risk of developing CRC, these include:
- Physical activity
- Diet- several changes in your diet can help to decrease in the development of CRC. It is recommended to consume foods high in:
- Fibre
- Folic acid
- Vitamin B6
- Calcium
- Dairy products
- Vitamin D
- Magnesium
- Garlic
- Fish
- Caffeine
- Drugs: certain drugs can help in the prevention of CRC such as:
- Aspirin
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
- Hormone therapy in women
- Statins
- Antioxidants
- Bisphosphonate
- Angiotensin 2 inhibitors

Prognosis
The approximate 5-year survival rate for CRC in people in the United States is 64%. Furthermore, as the stage of the disease increases, the 5-year survival rate drops significantly.

Source:
J. Alastair, I. and Simon, M., 2016. Davidson’s Essentials of Medicine. 2nd ed. London: ELSEVIER.
Parveen, K. and Michael, C., 2017. Kumar & Clarks Clinical Medicine. 9th ed. The Netherlands: ELSEVIER.
Dragovich, T., 2020. Colon Cancer




