What is coronary artery disease?
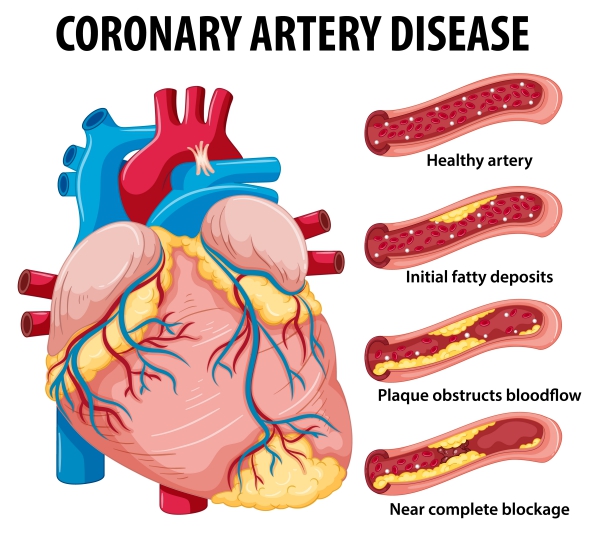
Coronary artery disease arise when the major blood vessels (coronary arteries) supplying the heart muscles with blood are narrowed or blocked. This most commonly happens due to the build-up of cholesterol on the wall of the coronary arteries, gradually narrowing the vessels and thus impairing the flow of blood to the heart. In some other cases, the blockage can be caused by a blood clot traveling from somewhere else in the body.
Coronary arteries are responsible for supplying the heart muscles with oxygen. When there is a restricted blood flow through these blood vessels, especially during physical activity, the heart will not have enough oxygen to perform its job properly, hence resulting in symptoms which can sometimes be severe. If there is complete blockage of the coronary arteries, you are at increased risk of having a heart attack.
Coronary artery disease is a very common condition in the United States, and it is also known to be the leading cause of death among both men and women. Approximately 14 million people experience coronary artery disease and its various complications in the U.S. There are several steps that can be taken to prevent or treat coronary artery disease.
Causes of coronary artery disease
Studies have shown that coronary artery disease usually arise from injury or damage found in the inner layer of the blood vessel. This damage increases the likelihood of the deposit of fat, forming up a plaque at the site of injury. This build-up is known as atherosclerosis. With time, these plaques can break off and dislodge, blocking smaller blood vessels. Platelets can also aggregate at the area where the plaque was located in an attempt to repair it, hence reducing your blood flow.

There are several factors that can cause damage in your blood vessels namely:
- Smoking
- High cholesterol in blood
- Being diabetic or having insulin resistance
- High blood pressure
- Having a sedentary lifestyle
You have four main coronary arteries which bring oxygen-rich blood to your heart muscles. Blockage of any of these vessels can lead to severe impairment. These are:
- Right main coronary artery
- Left main coronary artery
- Left circumflex artery
- Left anterior descending artery
Risk factors
Several factors can contribute in coronary artery disease and these are:
- High blood pressure: having a high blood pressure can contribute in changes in your blood vessel walls, favouring the narrowing of the arteries
- High cholesterol levels in the blood: having a high amount of cholesterol in your blood will precipitate the formation of plaques on your blood vessel walls. This is mainly caused by the bad cholesterol namely low-density lipoprotein (LDL). On the other hand, having not enough good cholesterol, high-density lipoprotein (HDL), can also favour atherosclerosis.
- Smoking: patients who smoke as well as those who breathe in second hand smoke are at increased risk of having coronary artery disease.
- Diabetes: if you have diabetes you have a higher risk of having coronary artery disease
- Family history: you are at higher risk of having coronary heart disease if you have a close relative who had the same condition at an early age.
- Sex: men are known to be at a higher risk compared to women. However, the risk increases in women after menopause.
- Overweight, obesity and physical inactivity
- Stress: stress can increase the damage to your blood vessels as well as worsening your other risk factors.

Signs and symptoms
You will start experiencing symptoms once your heart is not receiving enough oxygen-rich blood for it to function properly.
The most common symptom among patients with coronary artery disease is chest discomfort, also known as angina. Coronary artery disease can also present with an array of other symptoms such as:
- Chest pain: felt as a heavy or tight feeling on your chest. It is usually located in the middle or left side of your chest. Angina usually last for a few minutes after being triggered by physical activity and emotional stress.
- Shortness of breath: this is because your body is unable to pump enough blood to meet up your body’s demand. Therefore, any kind of exertion can become very tiring.
- Pain radiating to your arms and shoulders
- Sweating
 Feeling dizzy
Feeling dizzy- Weakness
- Nausea
- Development of abnormal heart rhythms
Making a diagnosis
Once you present with the above symptoms, your doctor will take a thorough medical history and examine you. Your doctor will also have to order certain tests to confirm the diagnosis of coronary artery disease.
These tests include:
- Electrocardiogram: this is a test done to record the electrical activity of your heart as well as its rhythm. It can show if there is an ongoing heart attack or if the patient had one in the past.
- Echocardiogram: this is a test done to visualize the structures of the heart by the use of sound waves.
- Stress test: this test is used to determine how your heart responds at rest and during physical activity. You will be required to walk on a treadmill or ride a stationary bike while having electrodes attached to your body. Your heart’s electrical activity will thus be recorded at the same time.
- Cardiac catheterization and angiogram: In this procedure, a catheter is inserted into your blood vessel and is guided to your heart with the help of X-rays. A dye is then injected and images taken to assess the flow of blood through your coronary arteries and to see whether there is the presence of any obstructions.
- Cardiac CT scan: If there are any calcium deposits in your arteries which are causing any narrowing, they will be visible using a cardiac CT scan.

Treatment of coronary artery disease
Lifestyle modifications play a significant role in modifying the course of the disease. It is very important for you to:
- Stop smoking and avoid second hand smoke
- Eat healthy- mainly decreasing your amount of fat intake
- Lose weight and start exercising- portion control and if you are currently physically inactive, it is advised for you to start slowly and gradually work your way up.
- Manage your stress with better coping strategies and relaxation therapies
In some cases, lifestyle modifications alone can be insufficient for your management. Your doctor will then prescribe you some medications to treat coronary artery disease, including:
- Cholesterol-modifying drugs: these drugs act by reducing the amount of cholesterol that can deposit on your blood vessels, especially low density lipoprotein. These drugs include statins, fibrates and bile acid sequestrants. These are especially important in patients with hyperlipidemia.
- Beta-blockers and angiotensin-converting enzyme inhibitors: this drug is necessary particularly if you have a high blood pressure and heart rate or if you already had a heart attack in the past.
- Aspirin: this drug helps to decrease the tendency of your blood to clot. This can also decrease your future risk of having a heart attack if you had one in the past.
- Nitroglycerin patches, spray or tablets: to control your chest pain by causing a temporary dilation of your coronary arteries.
- Calcium channel blockers: these drugs widen your coronary arteries to improve your blood flow in your heart muscles. It also acts by reducing the pressure of blood in your arteries

If your doctor sees that your condition is not improving only with medications and lifestyle modifications, some other procedures may be necessary. These include:
- Angioplasty and stent placement (percutaneous coronary revascularization): in this procedure, a catheter is inserted along the narrowed artery. A balloon is inflated through the catheter in the area of obstruction. This will compress the fatty deposits against the walls of the blood vessel, hence widening the artery.
- Coronary artery bypass surgery: in this procedure, a graft is used to bypass the blocked area in a blood vessel. This graft is obtained from another part of your body. This will create another pathway for your blood to flow, overriding the narrowing in your artery. This is an open-heart surgery and is mostly reserved for patients who have multiple areas of narrowing.
Complications
Coronary artery disease can lead to the following complications:
- Angina: chest pain and shortness of breath triggered by physical activity or emotional stress
- Heart attack: following complete occlusion of your coronary arteries. The lack of blood flow to your heart muscle leads to damage to your heart. The amount of damage is dependent on how quickly treatment was given to you.
- Heart failure: lack of oxygen-rich blood to your heart leads to muscular damage. This will prevent your heart form functioning properly to distribute blood throughout your body.
- Abnormal heart rhythm: damage to your heart muscles alter your heart’s electrical impulses.

Prevention
If you know that you are at increased risk of having coronary artery disease, some general changes can help you prevent ending up with diseased arteries namely:
- Exercising regularly
- Avoid alcohol intake
- Avoid tobacco smoke or quit smoking
- Decrease the amount of sugar, fat and salt in your diet
- Regularly check you levels of cholesterol in your blood
- Maintain a healthy weight
- Adopt proper stress management strategies
Prognosis
With proper prevention and management, coronary artery disease have a good prognosis. The earlier you start your management and lifestyle modifications, the better it is. However, it is important to know how it presents in order to properly recognise the condition, so that you seek medical help as soon as possible. You are advised to follow carefully your doctor’s instructions and take your medications properly.

Source:
J. Alastair, I. and Simon, M., 2016. Davidson’s Essentials of Medicine. 2nd ed. London: ELSEVIER.
Parveen, K. and Michael, C., 2017. Kumar & Clarks Clinical Medicine. 9th ed. The Netherlands: ELSEVIER.
Shah, S., 2019. Coronary Artery Atherosclerosis