What is Gastroesophageal reflux disease (GERD)?
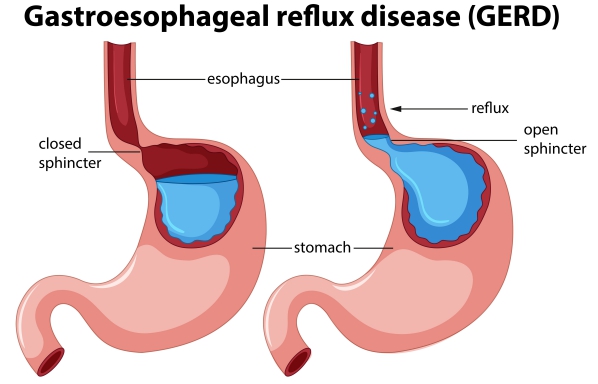
GERD, also known as acid reflux or regurgitation, is a condition in which the acid in your stomach flows back up into the digestive tube connecting the mouth to the stomach (esophagus). This results from the malfunctioning of the ring of muscles found at the junction of the esophagus and the stomach called the lower esophageal sphincter.
Normally, stomach contents should not flow back to the esophagus and the latter does not have to be in contact with stomach acid. Therefore, when this happens in GERD, the acid irritates the lining of the esophagus. Some people also call this condition heartburn, and this is something that we all experience from time to time. However, if this happens too often (about more than two times per week), you have what we call GERD.
Most of the time, GERD can simply be managed by some diet changes and lifestyle modifications. However, in a few cases, medications or even surgery may be required. If left untreated, this condition can lead to serious complications.
Causes of GERD
Normally, when you swallow, your food travels from your mouth, down your esophagus to then enter your stomach. Your lower esophageal sphincter relaxes to allow food and liquid to enter your stomach. Once this is completed, the sphincter closes to prevent the backflow of food and liquid into your esophagus.

If your sphincter is too weak to close properly, food contents along with stomach acid will flow back into your esophagus. This irritates the delicate lining of your esophagus causing inflammation. Another condition called hiatal hernia contributes in the development of GERD. Hiatal hernia is when the upper part of your stomach enters the chest cavity through a hole in your diaphragm which is a flat muscle separating the abdomen from the chest. This allows the acid contents from your stomach to flow back up more easily into your esophagus.
Risk factors for GERD
Besides anatomical problems, your choices in your diet and lifestyle highly contribute to GERD. For example, certain foods and drinks such as coffee, alcoholic drinks, fatty foods and chocolate may trigger the onset of acid reflux. Eating large meals and late at night or right before going to bed are known factors that contribute to GERD. Smoking and the use of nonsteroidal anti-inflammatory drugs (NSAIDS) such as aspirin or ibuprofen can also play a role in the symptoms of GERD. Being obese or pregnant also increases your risk of having reflux disease.
Signs and symptoms of GERD
GERD can present with the following signs and symptoms:
- Burning feeling in the chest (heartburn) moving up to the neck or throat
- Bitter or sour taste in the mouth
- Regurgitation of stomach food or liquid contents
- Relief of heartburn by standing upright or taking an antacid
- Difficulty to swallow
- Chronic cough especially if night time acid reflux

Since this presentation can be similar to the chest pain associated with heart disease, it is advised to seek medical help if you have chest pain as it is difficult to tell the difference.
Making a diagnosis
Your doctor will usually be able to make a diagnosis of GERD only with your history and physical examination. However, he/she may ask for some other tests to confirm the diagnosis or to check for the onset of any complications. These tests include:
- Barium swallow: In this procedure, you are asked to swallow a barium solution, followed by taking an X-ray of your digestive tract
- Upper endoscopy: Your doctor will use a thin tube equipped with a light source and a small camera (endoscope) to visualise your upper digestive tract. The endoscope is inserted through your mouth, down your throat and stomach. This allows visualization of any apparent inflammation of the esophagus. Other complications can also be diagnosed using this procedure. A small sample of the tissue found in your esophagus can also be taken to be examined. This is called a biopsy.
 Esophageal manometry: A tube is inserted in your esophagus to measure the force of contraction of the muscles found in there when you swallow.
Esophageal manometry: A tube is inserted in your esophagus to measure the force of contraction of the muscles found in there when you swallow.- Esophageal pH monitoring: A probe is placed in your esophagus to measure the pH changes inside whenever acid from the stomach regurgitates there.
Treatment of GERD
Initially your doctor would advise you to bring about dietary and lifestyle modifications as a first step in the management of GERD. The following can also be implemented if you want to prevent from having the condition.
These changes include:
- Avoid foods that can trigger reflux for example chocolate, coffee, mint, garlic, onion, tomato sauce, fatty and spicy foods and alcoholic beverages. Also avoid citrus foods and drinks as these may be causing symptoms.
- Eat smaller portions. Do not overeat and eat well before lying down or going to bed. It is advised to eat at least 2 to 3 hours before bedtime. Take your time to properly chew your food thoroughly and slowly.
- Stop smoking. It has been observed that smoking impairs the normal functioning of your lower esophageal sphincter.
- Maintain a healthy weight. Being obese will add pressure on your abdomen causing the stomach contents to flow up into your esophagus. Therefore, losing excess weight will help in alleviating your symptoms.
- Avoid wearing tight clothes. Similar to the effect of obesity, tight clothes will also be adding excess pressure on your stomach.
- Elevate the head of your bed. This makes use of the force of gravity to reduce the amount of reflux from your stomach. It is not advised to use multiple pillows in an attempt to elevate your head as this will worsen your symptoms.

If lifestyle and diet modifications are not enough to treat your GERD, your doctor can prescribe you some medications to alleviate your symptoms. These include:
- Antacids: these drugs neutralize the acid in your esophagus and stomach. In doing so, it relieves the burning sensation. They are available over-the-counter. However, this medication will not cure the damage and inflammation caused by the acid from the stomach. If taken too much, some unwanted side effects may arise such as diarrhoea or kidney problems.
- H-2-receptor blockers: these medications work by reducing the acid production in the stomach. Even if they do not provide relief as quickly as antacids, they provide relief of longer duration. These are also available over-the-counter, however, stronger versions of the drug are available as pre ion drugs. Examples include cimetidine, famotidine and nizatidine.
- Proton pump inhibitors: these work in almost the same way as H-2-receptor blockers, except that they are stronger in blocking the acid production. Hence, they give more time to the esophagus to heal from all the damage caused. Examples include omeprazole, lansoprazole or pantoprazole. Some side effects may include diarrhoea, headache, nausea and vitamin B-12 deficiency.

Most of the time, medications are sufficient in managing GERD. In some rare cases, surgery may be required. It is also useful in cases where you want to avoid long-term medications. The procedures include:
- Fundoplication: in this procedure, the stomach is wrapped around the lower part of the esophagus to strengthen it. This increases the pressure in the lower esophagus.
- Transoral incisionless fundoplication (TIF): this is done by a device inserted through the mouth. In this procedure, several folds are made around the junction of the esophagus and the stomach preventing reflux. As the name suggests, no incisions are required to undergo this surgery.
- Stretta procedure: an endoscope is used to create cuts at the base of the esophagus. When this will go through scarring, it will tighten the junction.
- Linx surgery: in this procedure, a ring of magnetic titanium beads (linx) is wrapped around the lower part of the esophagus.
Prognosis of GERD
Despite causing some impairment in everyday life, GERD is not a life threatening condition and can be easily managed. In very rare cases, GERD can lead to serious complications.
Complications of GERD
Rare complications include:
- Esophagitis: Inflammation of the esophagus
- Esophageal stricture: narrowing of the esophagus
- Barrett’s esophagus: this includes some permanent changes in your esophagus which increases your risk of having esophageal cancer
- Esophageal cancer
- Tooth enamel erosions and other dental problems due to the damage caused by acid regurgitation


Source:
J. Alastair, I. and Simon, M., 2016. Davidson's Essentials of Medicine. 2nd ed. London: ELSEVIER.
Parveen, K. and Michael, C., 2017. Kumar & Clarks Clinical Medicine. 9th ed. The Netherlands: ELSEVIER.
Kahrilas, P., 2020. Clinical manifestations and diagnosis of gastroesophageal reflux in adults
Kahrilas, P., 2020 Medical management of gastroesophageal reflux disease in adults