What is heart failure?
Heart failure occurs when your heart fails to pump the required amount of blood to all parts of your body. This condition is also known as congestive heart failure. There are certain conditions which may predispose you to heart failure, such as high blood pressure and coronary artery disease. Consequently, your heart becomes either too stiff or weak to pump blood effectively.
This condition can be acute or chronic and can occur in the right, left or both sides of the heart. In 2017, the American Heart Association (AHA) estimated that around 6.5 million Americans aged 20 years or older were affected by heart failure. In addition, men are more affected by heart failure than women.
Acute heart failure involves sudden onset of symptoms which may go away fairly quickly and often occurs as a result of a heart attack. However, in chronic heart failure, symptoms are ongoing and do not improve over time.
In heart failure, being a very serious medical condition, early treatment is essential to limit the occurrence of complications and increase your chance of long-term recovery. In addition to medical treatment, lifestyle modifications can also improve your quality of life.
What causes and risk factors of heart failure?
There are several causes and risk factors of heart failure and these include:

- Coronary Artery Disease (CAD): CAD is the most common cause of heart failure, in which your coronary arteries, the arteries which supply blood to your heart muscles, becomes narrow.
- Heart attack
- Congenital heart disease
- Cardiomyopathy: a condition that weakens your heart muscle.
- Heart valve disease
- High blood pressure
- Arrhythmias: abnormal heart rhythms may increase your risk of developing heart failure.
- Diabetes mellitus
- Emphysema: A disease that affects your lungs which places more stress on your heart to pump blood.
- HIV/AIDS
- Thyroid diseases
- Chemotherapy
- Severe anaemia
- Drug abuse
- Alcohol abuse
- Myocarditis
- Hemochromatosis: an abnormal build-up of iron in the body.
- Sleep apnoea: this is when you have difficulty breathing while sleeping at night.
- Viruses: viruses can infect and cause damage to your heart muscles
- Cigarette smoking
- Obesity
- Sedentary lifestyle
What are the types of heart failure?
Heart failure can be classified into right or left sided heart failure and systolic or diastolic heart failure:

- Left-sided heart failure: this is the most common type of heart failure. The left ventricle is the left lower chamber of your heart. It receives oxygenated blood from the lungs and is responsible for pumping blood to all parts of your body. When there is a valvular defect leading to your aorta, the largest artery in your body, there will be a reduced amount of blood reaching your organs and fluid accumulation into your lungs. This will make you feel breathless.
- Right-sided heart failure: the right ventricle is the right lower chamber of your heart which is responsible to pump deoxygenated blood into the lungs. When there is a left-sided heart failure or any valvular defects in the path leading to the lungs, the right ventricle has to pump harder to provide the lungs with sufficient blood. Consequently, this causes fluid accumulation in your lower extremities (pedal oedema) and abdomen (ascites).
- Systolic heart failure: this type of heart failure occurs when your heart muscle loses its ability to contract properly and is known as systolic dysfunction. This condition arises when your heart becomes weak and enlarged. It is also more common in men.
- Diastolic heart failure: this type of heart failure occurs when your heart muscle becomes stiff, preventing it from relaxing properly which will result in an inadequate filling of blood in your heart. This condition is also known as diastolic dysfunction. Consequently, there will be less blood reaching your organs. This type of heart failure is more common in women than in men.

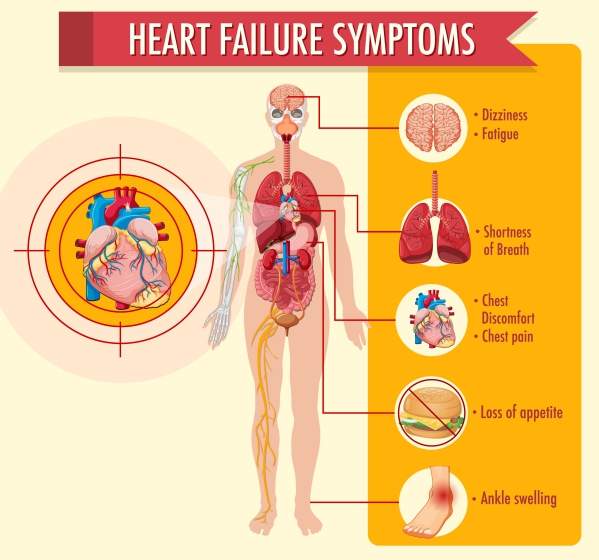
What are the signs and symptoms of heart failure?
The signs and symptoms of heart failure include:
- Pedal oedema
- Fatigue
- Difficulty breathing while lying down or after exertion
- Irregular heart beat
- Distended neck veins
- Reduced ability to concentrate
- Reduced ability to perform physical exercises
- Persistent productive cough with white, blood-tinged or pink frothy phlegm
- Distended abdomen due to fluid accumulation
- Loss of appetite
- Nausea
- Rapid weight gain from excess fluid accumulation
- Chest pain
Making a diagnosis
The diagnosis of heart failure starts by a thorough history taking by your doctor, during which he/she will ask you more about your symptoms. This is usually followed by a physical examination where your doctor will look for signs of heart failure. In addition, several tests can be performed to confirm the diagnosis of heart failure, such as:
- Electrocardiogram (ECG): this test assesses your heart function by measuring your heart’s electrical activities. In addition, your doctor will be able to identify any current or previous myocardial infarction and assess the rhythm of your heart.
- Blood tests: several blood tests can be performed to help in the diagnosis of heart failure, such as:

- Cardiac Troponin I and T: these are usually elevated after a myocardial infarction.
- Complete blood count: this test is used to rule out anaemia or any infection.
- Urea, electrolytes and creatinine levels: these tests are mainly used to assess your renal function.
- Liver function test: to assess the function of the liver as it is usually congested in heart failure.
- Fasting blood glucose
- Brain natriuretic peptide: this is usually elevated when your heart is not functioning properly.
- Chest X-ray: this is done to differentiate between a heart or lung problem. In heart failure, the heart can be enlarged which will be identified on X-ray. Furthermore, the accumulation of fluid inside or around your lung can also be identified.
- Echocardiography: it is mainly done to identify the potential cause of the heart failure by assessing the heart chambers, valves and muscle wall motion.
- Exercise test or stress test: in this test, electrodes are used to measure your heart’s electrical activity while you run on a treadmill. This is to identify any abnormality which is associated with exertion.
Treatment of heart failure

Lifestyle modifications such as avoiding alcohol, smoking cessation, maintaining a healthy weight and eating less salt may help in the management of heart failure. The treatment mainly focuses on treating the causes of heart failure. In addition, your doctor will prescribe medications such as:
- Diuretics: these drugs help to remove excess fluid from your body. A commonly used diuretic is furosemide.
- Angiotensin Converting Enzyme (ACE) inhibitors: ACE inhibitors help to dilate your blood vessels thus increasing the amount of blood going through your heart and lowering your blood pressure. Examples include enalapril and Lisinopril.
- Beta blockers: these drugs lower your blood pressure which decrease the mortality rates and improve your symptoms. However, it should be started on a low dose.
- Mineralocorticoid receptor antagonist: this drug improve your kidney’s ability to excrete excess fluids from your body.
- Digoxin: it helps to improve your symptoms by increasing the force of contraction of your heart.
- Vasodilators: these dilate your blood vessels and lower your blood pressure.
Pacemakers can be used in people who are having abnormal heart rhythms. Furthermore, Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) are not to be used by people suffering from heart failure.
Complications of heart failure
Complications of heart failure include:
- Heart valve disorders
- Kidney injury or failure
- Liver congestion and dysfunction
- Abnormal heart rhythm
- Stroke
- Pulmonary embolism
- Deep vein thrombosis
- Pulmonary congestion and hypertension
- Muscle wasting

Prevention of heart failure
Heart failure can be prevented by reducing risk factors. Several lifestyle modifications can be adopted to prevent heart failure, such as:
- Smoking cessation
- Avoiding alcohol consumption
- Managing stress effectively
- Eating a healthy diet
- Doing regular physical exercises
- Keeping a healthy weight
- Controlling your hypertension and diabetes
Prognosis
Unfortunately heart failure has a poor prognosis. 25-50 % of people suffering from heart failure die within 5 years of diagnosis. Therefore, it is of utmost importance to seek medical help as early as possible to prevent you from suffering from heart failure.

Source:
J. Alastair, I. and Simon, M., 2016. Davidson’s Essentials of Medicine. 2nd ed. London: ELSEVIER.
Parveen, K. and Michael, C., 2017. Kumar & Clarks Clinical Medicine. 9th ed. The Netherlands: ELSEVIER.
Oxford handbook of Clinical medicine, 10th edition.
Dumitru, I., 2020. Heart Failure


