What is Lyme disease?
Lyme disease is an infection affecting various organ systems in the body which is caused by a pathogen known as Borrelia burgdorferi. It is an infection that is transmitted through tick bites. It is the most common cause of vector-borne illness in the United States and Europe and there is more than 30,000 cases reported each year according to the Centers for Disease Control and Prevention. It is particularly common in people who spend a lot of time outdoors and in forested, brushy areas. Besides being present in grass and forest, the ticks are also carried by mice, birds and deer.
The cycle of infection of the Borrelia burgdorferi pathogen starts when it colonizes Ixodes ticks. The infection is then transmitted to a variety of mammals, including humans through tick bites. The life cycle of these ticks can last for around 2 years. The ticks need to be attached to the skin for about 36-48 hours before transmission of the pathogen occurs. Infection with Borrelia burgdorferi usually occurs in late spring and summer. The symptoms usually arise within a few days or weeks after the tick bites.
In most cases, antibiotics are very effective in the treatment of Lyme disease and helps in the elimination of symptoms as well as preventing the progression of the disease. The time taken for the symptoms to disappear varies.
 What are the risk factors of Lyme disease?
What are the risk factors of Lyme disease?
You are at increased risk of having Lyme disease if you:
- Spend a lot of time outdoors such as working outdoors, in the garden or participating in activities including hunting and hiking
- Live in areas near old stone walls or between forest land and lawns and low-lying shrubs or grasses
- Have close contact with pets as the ticks can attach to them

What are the symptoms of Lyme disease?
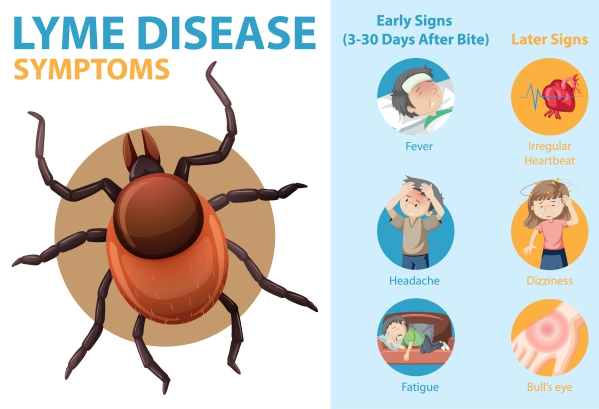
The clinical presentation of Lyme disease varies from person to person as it involves multiple organ systems. The symptoms arise as a result of the response of your immune following the tick bite and the inflammation associated with it. The symptoms vary according to the phase of the infection. It can be divided into 3 phases namely early localised, early disseminated and late Lyme disease.
Early localised
In the early phase, Lyme disease can cause local changes where the tick bite has occurred. This is a skin condition known as erythema migrans. It usually appears within the first month of the tick bite. It appears as a skin rash at the biting site. It is commonly salmon to red-coloured covering the entire lesion (majority of cases) or it may have a clear centre giving it a “bull’s-eye” appearance.

Tick bites most commonly occurs in the armpit, groin area, back of the knees or the belt line. The lesion usually itches or burns and can expand with time. Other symptoms that may be associated with this stage include fatigue, malaise, fever, headache, muscular pain, joint pain and swollen lymph nodes.
Early disseminated disease
In this stage, the bacteria causing Lyme disease spreads into the bloodstream and travels to other areas of the body. This result in inflammation in various organ systems. It can occur within days to weeks after the tick bite. The symptoms can be classified as the following:
- Cardiac symptoms: In some cases, inflammation of the heart may occur, especially if Lyme disease is left untreated. Heart blocks may occur which is due to inflammation interrupting the normal electrical impulse conduction. This results in a slower heart rate, light-headedness and fainting. In some people, this may result in no symptoms at all.
- Neurologic symptoms: If the inflammation reaches the nervous system, the following symptoms may occur: headache, neck stiffness, weakness, pain and numbness.
Late disease
In this stage of the disease, the inflammation affects joints, nervous system and the skin. These can arise months to years after a tick bite.
- Muscle and joint symptoms: These symptoms occur in the majority of people in whom the infection has been left untreated. These symptoms include joint pain and joint inflammation (also known as arthritis).
- Neurologic symptoms: These symptoms include pain, impaired memory or thinking and numbness.
- Skin symptoms: With time, skin nodules, swelling and thinning of skin may occur.

How is the diagnosis of Lyme disease made?
To make the diagnosis of Lyme disease, your doctor will first take a thorough history from you focusing on any possible exposure to tick bites. He/she will then proceed with examining you. The following tests may help your doctor to confirm the diagnosis:
- Blood tests: Blood tests are available to check for current or previous infection with Borrelia burgdorferi pathogen. These tests include enzyme-linked immunosorbent assay (ELISA) and Western blot. They detect the presence of antibodies against the bacteria. Antibody tests, however, are not reliable in early stages of the disease.
- Cerebrospinal fluid tests: If you have neurologic symptoms and the diagnosis is doubtful, your doctor may take a sample of your cerebrospinal fluid (fluid surrounding the brain and spinal cord) for further analysis to confirm the diagnosis. This is collected through a procedure known as a lumbar puncture. In this procedure, a needle is inserted in your back under local anaesthesia. A small sample of the cerebrospinal fluid is collected in a collecting tube.
 How is Lyme disease treated?
How is Lyme disease treated?
The mainstay of treatment for Lyme disease is antibiotics. However, it depends on the stage of the disease as well as the symptoms present. Recovery may take weeks to months after having completed the treatment course. In some cases, initiation of treatment may trigger a brief worsening of symptoms also known as a Jarisch-Herxheimer reaction. This may occur within the first 24 hours of treatment and resolve within a few days. You should not stop the antibiotic course even if this happens.
The antibiotics usually used include doxycycline, amoxicillin or cefuroxime. Normally, oral antibiotics are prescribed. However, if the infection is severe and especially affects the brain, intravenous antibiotics may be needed.
It is possible that you get the infection again after being treated if you get bitten by another infected tick. However, this occurs rarely as your body develops a stronger and longer-lasting antibody response.
How can Lyme disease be prevented?
The following measures can help to prevent you from having Lyme disease:
- Wear protective clothing to keep ticks away. You may also pre-treat your clothing with permethrin to further reduce the risk.
- Shower within 2 hours of having potentially be exposed to ticks.
- Use tick repellents or tick-killing products containing active ingredients such as DEET, IR3535 or picaridin.
- Inspect your clothes and skin after having been outdoors.
Source:
Mead, P., and Schwartz, A., 2020. Epidemiology of Lyme disease
Hu, L., 2020. Clinical manifestations of Lyme disease in adults
Hu, L., 2020. Diagnosis of Lyme disease
Hu, L., 2020. Treatment of Lyme disease
Meyerhoff, J., 2019. Lyme Disease





