What is malaria?
Malaria is an infectious disease that is caused by a parasite known as Plasmodium protozoa, transmitted by bites from the female Anopheles mosquito. It is a disease that is most common in tropical areas and can be potentially life-threatening. Malaria can be caused by 5 types of Plasmodium species. It is important to identify the one causing the disease as some species may be resistant to certain treatments and eventually be fatal, for example infection with P falciparum. 5-7% of people with malaria are infected with more than one species of Plasmodium.
Malaria is most common in the following regions: Central America, South America, Hispaniola, sub-Saharan Africa, the Indian subcontinent, Southeast Asia, the Middle East, and Oceania. However, sub-Saharan Africa remains the area with the highest transmission of P falciparum. Malaria causes around 1-3 million deaths per year, with 300-500 million of new cases annually.
The disease affects men and women equally. However, malaria during pregnancy can be devastating as it can cause maternal or fetal complications or death.
What are the causes and risk factors of malaria?
As mentioned above, malaria is an infectious disease caused by the Plasmodium protozoa species. It is transmitted through mosquito bites in endemic areas. You are more at risk of having the disease if you have not taken the necessary precautions while living in a malaria prone area such as use of bed nets, diethyl-meta-toluamide (DEET) and appropriate use of malaria prophylaxis before travelling.

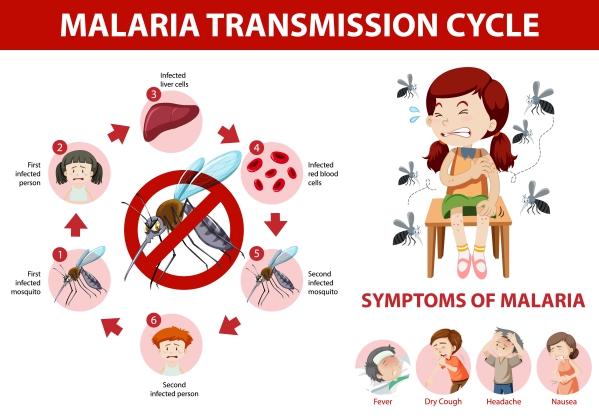
Once the mosquito bites a host, the parasite travels to the liver of the person within minutes. After a few weeks, the parasite migrates in the bloodstream of the infected individual. It then invades the red blood cells in the bloodstream where they further mature. When the red blood cells rupture, symptoms begin to appear. The parasites leave the ruptures red blood cells to invade healthy ones. The cycle starts all over again when a mosquito bites the infected individual and transmits it to a healthy person. Plasmodium is unlikely to be transmitted through blood transfusions or through maternal-fetal transmission.
The course of the disease depends on each person’s immune system. Some people with a well-functioning immune system may easily clear the infection while in others, the infection progresses. Malaria from the P falciparum species may result in death.
What are the symptoms of malaria?
Malaria can present with the following symptoms:
- Cough
- Malaise
- Weakness and fatigue
- Chills
- Joint pain
- Muscular pain
- Fever spikes
- Increased sweating
- Loss of appetite
- Nausea and vomiting
- Yellowing of skin known as jaundice
- Diarrhoea
The following symptoms are present in complicated malaria:
- Coma
- Seizures
- Confusion and drowsiness
- Severe anemia
- Decreased urine output
- Difficulty in breathing

How is the diagnosis of malaria made?
To make the diagnosis of malaria, your doctor will first start by asking you a series of questions. These will include questions about recent travel to endemic areas and questions about your general health.
The main tests done to confirm the diagnosis are blood tests. Blood samples are taken to check for the presence of the parasite under a microscope. The type of parasite present is also identify to guide treatment as certain strains may be resistant to particular medications.
Other tests may be requested to identify the presence of any possible complications.
How is malaria treated?
The treatment of malaria is targeted to eradicate the parasites present in the body. There are anti-malarial medications available for the treatment of malaria. The choice and length of treatment depends on the type of parasite, severity of symptoms, age as well as pregnancy status. Treatment options include:
- Artemisinin-based combination therapies (ACTs): These medications work by killing the parasites in the body and are available in the form of tabs. They are usually the first drugs to be chosen for the treatment of malaria. Some examples include: artemether-lumefantrine and artesunate-amodiaquine. In severe malaria, the medications may have to be delivered directly through your veins.
- Chloroquine phosphate: This medication is the one preferred for any parasite that is not resistant to it. P falciparum is resistant to chloroquine and therefore is no longer considered as an effective treatment.

How can malaria be prevented?
When you are planning to travel to a malaria-prone area, it is recommended to take the necessary precautions. A prophylaxis is a medication or a measure taken to prevent the occurrence of a disease. The choice of the prophylactic agent that is best for you will depend on the risk of malaria in the area you are visiting as well as the degree of resistance to chloroquine present in that country. Some prophylactic agents include the following: chloroquine, atovaquone plus proguanil, doxycycline and mefloquine. Once arrived in the area to be visited, it is recommended to make use of mosquito bed nets or insecticide treated bed nets, insect repellents and protective clothing to prevent mosquito bites. There are no vaccines available for malaria.
Complications of malaria
Malaria has shown to be associated with the following complications:
- Accumulation of fluid in the lungs known as pulmonary edema
- Rapidly progressing anemia due to rupture of red blood cells
- Renal problems
- Obstruction of small blood vessels
- Seizures
- Coma
- Confusion
- Decrease in blood sugar levels
- Bleeding disorders

Prognosis
In uncomplicated malaria, initiation of treatment can lead to significant improvement within the first 48 hours and no longer have fever after 96 hours. Malaria caused by P falciparum is associated with a poorer outcome and higher mortality rate. However, if early diagnosis is made and appropriate treatment is initiated the earlier possible, the outcome is excellent.

Source:
Herchline, T., 2020. Malaria Treatment & Management
Herchline, T., 2020. Malaria
Hopkins, H., 2020. Laboratory tools for the diagnosis of malaria
Breman, J., 2020. Malaria: Epidemiology, prevention, and control
Breman, J., 2020. Malaria: Clinical manifestations and diagnosis in nonpregnant adults and children