What is mesenteric ischemia?
Mesenteric ischaemia is a condition that occurs when there is restricted blood supply to your small intestines due to narrowed or blocked blood vessels. Prolonged reduction in blood supply to your small intestines can permanently damage it. When there is sudden loss of blood flow to your small intestines due to a blood clot, this condition is known as acute mesenteric ischaemia which requires immediate surgery to restore the blood supply. On the other hand, when mesenteric ischaemia occurs progressively over time, it is known as chronic mesenteric ischaemia which is treated with open surgery or angioplasty- a procedure to restore blood flow through an artery using a thin tube which is inflated to increase the diameter of the affected blood vessel. If this condition is left untreated, it can be life-threatening.
In the United States, the risk factors for acute mesenteric ischaemia are atherosclerosis (the build-up of plaque inside an artery resulting in a narrowed blood vessel), irregular heart rhythm, congestive heart failure, advanced age and cancer inside the abdomen.
What are the causes and risk factors for mesenteric ischaemia?
Acute mesenteric ischaemia is mainly caused by a reduction or complete cessation of blood flow to your small intestines due to blood clots. The blood clot may be formed elsewhere and gets lodged in the intestinal blood vessels and this is known as embolism. The blood clot may come from the heart due to irregular heartbeats (arrhythmias) or dysfunctional heart valves. On the other hand, the blood clot may form in the intestinal blood vessel itself causing a reduction or complete cessation of blood flow and this is known as thrombosis. The thrombosis may be caused by atherosclerotic vascular disease, aortic aneurysm (this is when your aorta is enlarged due to a weakened arterial wall), arteritis (inflammation of your arteries) or severe dehydration.

Other risk factors include a hypercoagulability state (a high probability of forming blood clots inside blood vessels), inflammation of the pancreas (pancreatitis), decompression sickness, appendicitis or trauma to blood vessels due to accidents or surgery.
What are the signs and symptoms of mesenteric ischaemia?
The signs and symptoms of mesenteric ischaemia varies and depends on whether it is acute or chronic. The signs and symptoms of acute mesenteric ischaemia include:
- Fever.
- Nausea.
- Vomiting.
- Sudden, severe abdominal pain.
- Urgent need to have a bowel movement.
- Diarrhoea.
- Loss of appetite.
- Rectal bleeding (due to a gangrenous small intestine).
- Low blood pressure.
- Altered mental status.
- Increased heart rate.
- Increased respiratory rate.
- Unexplained weight loss.
The signs and symptoms of chronic mesenteric ischaemia include:
- Fear of eating.
- Abdominal pain after eating.
- Diarrhoea.
- Nausea.
- Vomiting.
- Constipation.
- Flatulence.
There are some diseases which may resemble mesenteric ischaemia and these include:
- Ovarian torsion.
- Crohn’s disease.
- Volvulus.
- Hepatic disease.
- Abdominal abscess.
- Acute abdomen.
- Abdominal aortic aneurysm.
- Acute pancreatitis.
- Appendicitis.
- Bacterial sepsis.
- Biliary disease.
- Ectopic pregnancy.
- Intestinal perforation.
- Diverticulitis.
- Nephrolithiasis.
- Septic shock.
- Small bowel obstruction.
- Myocardial infarction.

Making a diagnosis
To make a diagnosis, your doctor will first take a detailed history from you to know more about your symptoms. After the history taking, your doctor will perform a thorough physical examination to look for signs of mesenteric ischaemia. To confirm the diagnosis, your doctor will order some tests and these include:
- Laboratory tests: Laboratory tests are nonspecific and unreliable but can help to rule out other conditions and these include prothrombin time (PT)m activated partial thromboplastin time (aPTT), international normalized ratio (INR), complete blood count and lactate dehydrogenase (LDH) levels.
- Plain abdominal radiography: This imaging technique is only useful in 30% of cases and therefore should not be used to rule out mesenteric ischaemia. However, it can be used to rule out other conditions such as a perforated bowel.
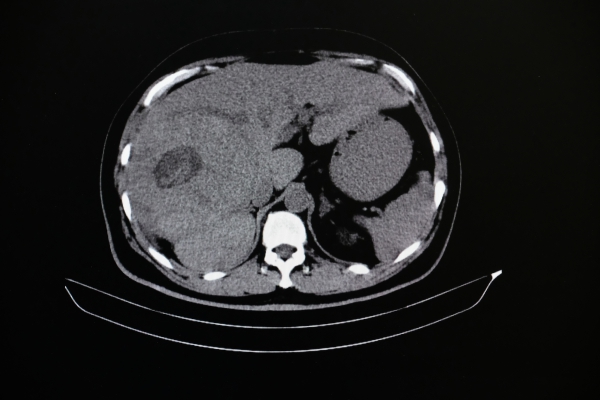
- Angiography: Angiography is an imaging technique that produces images of your blood vessels to determine if they are narrowed. There are different types of angiograms which can be used such as Computed tomography (CT) angiogram and Magnetic resonance imaging (MRI) angiogram.
- CT and MRI scans of the abdomen: CT and MRI scans of the abdomen are very valuable as they allow detailed examination of the small intestines and intestinal blood vessels.
- Doppler ultrasonography: This imaging technique is a noninvasive test that uses sound waves to estimate blood flow in the blood vessels and determine if they are narrowed.

What are the treatments of mesenteric ischaemia?
The initial step in the management of mesenteric ischaemia is to improve the blood supply to the bowels using medications. Papaverine is an infusion which is relaxes the artery which is affected to improve the blood supply. Thrombolytics agents are medications which help to dissolve the blood clot blocking the bloodstream. However, thrombolytics can cause bleeding if not used properly. Heparin is an anticoagulant, that is, it prevents the formation of blood clots. If the intestines are not yet in the process of degradation, using heparin may even make surgery unnecessary.
Before surgery is done, the person should be stabilized using the above medications. After being stabilized, your surgeon may perform a surgery to remove the nonviable sections of the bowel and restore the blood supply. However, in chronic mesenteric ischaemia, your surgeon may insert a catheter which can be inflated into the affected blood vessel to open the narrowed area. In addition, a stent may be placed in the narrowed area to keep the blood vessel open.
What are the complications of mesenteric ischaemia?
If acute mesenteric ischaemia is left untreated, the following complications may ensue:

- Sepsis: Acute mesenteric ischaemia can lead to infection and eventually to sepsis. Sepsis is the body’s extreme response to an infection and is a life-threatening medical emergency. The chemicals released by the body into the bloodstream to fight the infection can trigger changes that can lead to multiple organ failure.
- Irreversible intestinal damage: Insufficient blood supply to the intestines may cause death to that part of the intestine which needs to be removed through surgery.
- Death: Both sepsis and intestinal damage can lead to death if left untreated.
It chronic mesenteric ischaemia is left untreated, the following complications may ensue:
- Fear of eating: Due to after-meal pain associated with chronic mesenteric ischaemia, the affected person may be afraid to eat to avoid the pain.
- Unintentional weight loss: This may occur as a consequences of fear of eating.
- Acute-on-chronic mesenteric ischaemia: Chronic mesenteric ischaemia can progress and lead to acute mesenteric ischaemia.
Expectations (prognosis)
Over the past 15 years, the mortality rate from acute mesenteric ischaemia is 71% and once the affected part of the intestine dies, the mortality rate rise to 90%. However, early and aggressive diagnosis and treatment have helped to decrease the mortality rate. People affected by chronic mesenteric ischaemia suffer from malnutrition in the long run due to the fear of eating.


Source:
J. Alastair, I. and Simon, M., 2016. Davidson's Essentials of Medicine. 2nd ed. London: ELSEVIER.
Parveen, K. and Michael, C., 2017. Kumar & Clarks Clinical Medicine. 9th ed. The Netherlands: ELSEVIER.
Alrayes, A., 2019. Chronic mesenteric ischaemia.
Dang, C., 2020. Acute mesenteric ischaemia.
Sachs SM, Morton JH, Schwartz SI. Acute mesenteric ischemia. Surgery. 1982 Oct. 92(4):646-53.
Moawad J, Gewertz BL. Chronic mesenteric ischemia. Clinical presentation and diagnosis. Surg Clin North Am. 1997 Apr. 77(2):357-69.
Jaster A, Choudhery S, Ahn R, et al. Anatomic and radiologic review of chronic mesenteric ischemia and its treatment. Clin Imaging. 2016 Sep-Oct. 40(5):961-9.
Patel R, Waheed A, Costanza M. Chronic mesenteric ischemia. StatPearls. 2019 May 11.