What is Migraine?
Migraine is a disorder that causes recurrent and severe pulsating pain in your head, usually located on only one side. It can be accompanied by other symptoms such as visual and sensory disturbances. The latter are known as aura and can occur before or during the headache.
Migraine is complex and is one of the most common reason people seek medical help. It is estimated that more than 30 million people in the United States have 1 or more migraine each year. It is more common among women. The World Health Organization (WHO) estimates that around 10% of the world’s population have migraine.
Headaches can be severe in some cases. However, most of them are not due to an underlying life-threatening disorder. Treatment of migraine depends on the type and severity of the condition.
Causes of Migraine
The exact cause of migraine is not completely understood. However, it has been shown that certain factors such as genetics and environmental factors may contribute.
About 70% of people having migraine have a first degree relative with a history of the same condition. Studies have identified certain genes that could possibly be associated with the inheritance of migraine. Other factors may trigger migraines including:
- Changes in hormones, for example, associated with menses, pregnancy or ovulation
- Stress
- Too much or not enough sleep
- Certain medications such as oral contraceptives
- Smoking
- Exposure to bright light
- Some strong odours such as perfumes or petroleum products
- Trauma to the head
- Changes in weather
- Motion sickness
- Lack of physical activity
- Red wine

Certain food or food additives may also be associated with precipitation of migraine such as:
- Caffeine
- Artificial sweeteners
- Monosodium glutamate
- Citrus fruits
- Meats containing nitrites
Risk factors for migraine
Some factors can increase your risk of having migraine including:
- Obesity
- High blood pressure
- High cholesterol levels
- Diabetes
- Stroke
- Coronary heart disease
- Increase in inflammatory markers
- Family history of migraine
- Increased aged
- Female gender
Signs and symptoms
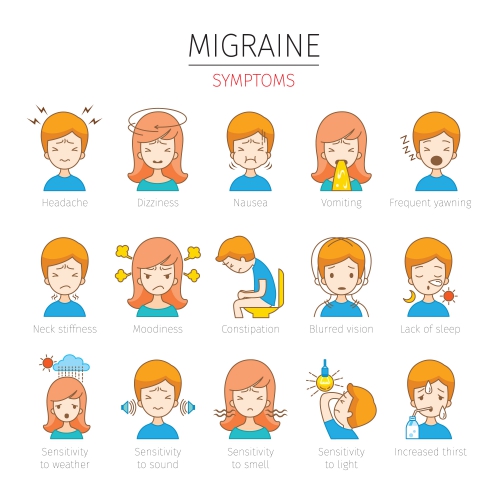
Migraine can be classified into migraine without aura or migraine with aura. Both present with the following symptoms:
- Pulsating or throbbing pain on one side of the head
- Headache aggravated by sneezing, straining or motion
- Nausea
- Vomiting
- Light-headedness
- Increased sensitivity to light
Around 60% of people may experience some other premonitory symptoms prior to the migraine attack. These symptoms can occur hours to days before the onset of headache. These symptoms may include:

- Increased sensitivity to light, sound or odours
- Fatigue
- Food cravings
- Mood lability including depression, euphoria or anger
- Increased thirst
- Loss of appetite
- Constipation or diarrhoea
- Neck stiffness
Migraine with aura, as the name suggests, presents with aura symptoms which includes:
- Flashing lights
- Seeing bright spots or zigzag lines
- Numb or tingling fingers or areas of the face
- Muscle weakness
- Loss of vision
- Loss of sensation in limbs and face
- Speech and language disturbances
Symptoms of migraine may relieve by lying down in a dark and quiet room. The symptoms may last for hours or even days.
Making a diagnosis
Normally, a good history and physical examination is enough to make the diagnosis of migraine. In some cases, further investigations may be required to:
- Exclude other causes of headache that mimic migraine
- Rule out other diseases that can possibly make migraine worse
- Exclude any factors that can affect the choice of treatment
- Measure the levels of migraine medications in your blood to check for how well it is working and whether you are complying with the treatment prescribed.
Special imaging techniques that may be required for the above reasons may be a magnetic resonance imaging (MRI) or a computed tomography (CT) scan. These allow detailed visualisation of the brain and identification of any possible abnormalities causing headache. Some indications for imaging may include:

- Having a first or worst headache ever
- Change in pattern of usual migraine
- Abnormal neurologic findings on your physical examination
- Onset of migraine after 50 years of age
- Presence of fever
- Presence of seizure
Treatment of Migraine
The choice of treatment for migraine depends on the frequency, severity or symptoms of your migraine. Treatment may be classified into acute or preventive treatment. Acute treatment includes medicines taken to alleviate migraine immediately while preventive treatment includes medications that are taken regularly to prevent future migraines.
Acute treatment
Medications included in the acute treatment of migraine include the following:
- Pain relievers: Some migraines may respond favourably to pain relievers, most of which are available without any pre ion. Some examples include aspirin, acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs). In some cases, pain relievers combined to caffeine may be given to improve its efficacy. The above medications are the first recommended for mild to moderate attacks. However, if overused, they can often lead to chronic headache. If you have gastritis, ulcers, kidney disease or bleeding disorders, you should not be taking medications containing aspirin or NSAIDs.
- Triptans: In some cases, pain relievers may be of no use in controlling your headache. Therefore, your doctor will recommend you to switch to Triptans which are migraine-specific medications. Some examples include sumatriptan, zolmitriptan, naratriptan and rizatriptan. Triptans are available in the form of oral pills, sprays or injections. Your doctor will advise you on the best mode of administration for you. These medications should also be used in moderation as overuse can lead to chronic headaches.
- Anti-nausea medications: If your migraine is accompanied by nausea or vomiting, your doctor may recommend you to use anti-nausea medications either intravenously or by injection. Some examples include metoclopramide, chlorpromazine or prochlorperazine.
- Lasmiditan: This is a new medication for migraine. It can be an alternative for people who should not be taking Triptans due to other coexisting medical conditions. Some side effects of the drug include dizziness, fatigue, tingling sensation in your limbs and nausea. You should avoid driving for at least 8 hours if you take this medication.
- Ergots: These are migraine-specific medications. Some examples include dihydroergotamine and ergotamine. Ergots are not as effective as Triptans and are associated with more side effects. If you have high blood pressure, coronary artery disease, kidney or liver disease, you should not be taking ergots.
- Dexamethasone: Dexamethasone is a steroid medications that can reduce the risk of recurrence if given along with migraine medications.

Preventive treatment
Preventive treatment include the following:
- Lifestyle changes: Staying consistent with bedtimes and wake times, avoiding alcohol and caffeine, avoiding smoking before going to bed and limiting your screen time right before bed can all help in preventing migraine attacks. It is also recommended that you eat healthy meals and exercise regularly.
- Beta blockers: These medications, usually used to treat high blood pressure, has been shown to be effective in the prevention of migraine attacks. Some examples include metoprolol, propranolol and timolol.
- Antidepressant medications: Some antidepressant medications are recommended in the prevention of migraine attacks, including amitriptyline, nortriptyline and doxepin.
- Anti-seizure medications: Valproate and topiramate has shown to be effective in the prevention of migraine attacks. However, both medications are associated with side effects. Women who are pregnant or planning to become pregnant should not be taking these medications as they can lead to birth defects.
- CGRP antagonists: These medications work by blocking the pain pathway and these are usually used in people who cannot find relief from the above medications. Some examples include erenumab, fremanezumab, and galcanezumab.
- Calcium channel blockers: Calcium channel blockers are medications mostly used for treating high blood pressure. They are also prescribed as a medication to prevent migraine attacks. Some examples include verapamil and nifedipine.

Complications of migraine
Migraine can lead to complications with time. Some of the complications include:
- Chronic migraine
- Seizures provoked by migraine
- Stroke with migraine
- Persistent aura symptoms
Stroke, despite being a rare complication, can be very serious. Factors that increase the risk of having a stoke with migraine include
- Migraine with aura
- Being female
- Cigarette smoking
- Oral contraceptive use (Estrogen)
Prognosis
Despite being a chronic disorder, prolonged periods of remissions occur frequently. Many people may have complete remission while others may only have partial remissions. With appropriate treatment, severity of migraines can significantly be reduced.

Source:
Chawla, J., 2020. Migraine Headache.
Cutrer, M., 2019. Pathophysiology, clinical manifestations, and diagnosis of migraine in adults.
Smith, J., 2020. Preventive treatment of migraine in adults.