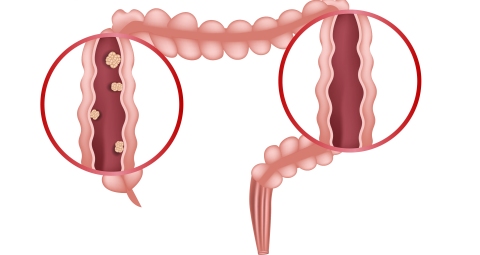
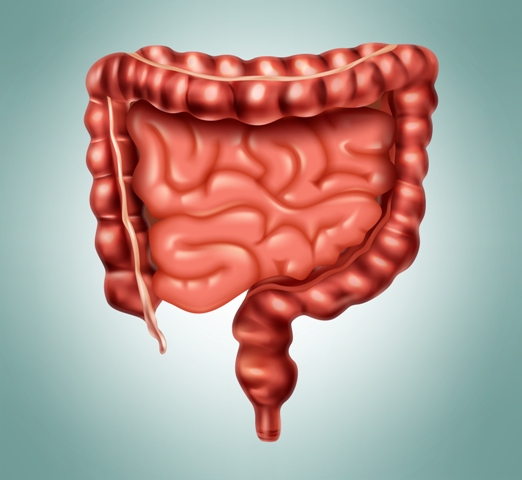
Diverticular disease is a pathological condition in which abnormal pouches are formed within the lining of colon. These small pouches or small mucosal sacs are known as diverticula and these are protruded through the intestinal wall
Basically prolong history of constipation is considered as one of the most important causes of diverticular disease because constipation is accountable for increasing intracolonic pressure, which ultimately leads to rupturing of the bowel wall especially at the weak points as a result small pouches or pockets are produced, which are termed as diverticula
Presence of diverticula within the colon is medically known as diverticulosis and if the diverticula get inflamed and infected then such condition is termed as diverticulitis.
Diverticulitis is very severe in its manifestation. It may cause severe abdominal cramping, fever as well as nausea. Over growth of microbes within diverticula may leads to diarrhoea as well. Diverticulitis requires instant medical supervision due to various complications like ulceration, bleeding, perforation etc.
It is always better to prevent diverticular disease or diverticulosis at early stage for avoiding further life threatening complications
Causes
The exact cause of diverticular disease are not certain. Some studies have shown that hereditary factors are responsible for developing diverticular disease. Whereas as per various other studies below stated factors are considered as the leading causes of diverticulasr diseases –
- The movement of hard stool through the colon
- Prolong consumption of low fibre diet
- Excessive consumption of fatty and spicy food
- Low intake of water
- Anatomical defects
- Aging (it is very prevalent after the age group of 40)
- Poor physical activity
- Smoking cigarettes
- Alcoholism
- Prolong consumption of some drugs such as opioids, steroids, nonsteroidal anti-inflammatories drugs etc


Signs and symptoms
- Chills
- Fever
- Severe abdominal pain
- Nausea
- Vomiting
- Constipation
- Rectal bleeding
- Changes in bowel pattern
These are the common symptoms, which are experienced by people with diverticular disease
Complications
Individual with acute diverticular disease, develop various complications, which include –
- Formation of fistula (an abnormal passageway) between the bowel and other organs
- Blockage in the bowel due to scarring
- An abscess, which is occurred when pus get accumulated within the pouch
- Peritonitis is a severe complication of diverticular diseases, when the inflamed or infected pouch ruptures then the intestinal content spill out within the abdominal cavity, which leads to peritonitis. It may cause sepsis as well. Peritonitis is a life threatening complication and it requires immediate medical care

Nutritional management
Nutrition is considered as the primary consideration for preventing and treating diverticular disease. An increase intake of fluid as well as fibre must be emphasized and low intake of fat is also suggested
In mild symptoms a clear fluid diet is recommended for promoting the recovery whereas in severe condition hospitalization is required for providing intravenous feeding in order to provide proper rest to the bowel
Below points will provide a dietary guideline, which should be followed for improving the symptoms of diverticular disease –
Energy
- Energy should be consumed as per RDA
- We know that carbohydrates and fats act as the main sources of energy whereas proteins are utilized for anabolic functions
- In this condition it should be kept in mind that maximum of the daily energy need should be fulfilled from carbohydrates, not from fats because excessive fat consumption is not safe
Carbohydrates
- It is better to focus on the consumption of complex carbohydrates as they contain enough fibres and fibres are considered as one of the most important nutrients required for treating diverticular disease
- Fibre plays vital role in making the stool soft by increasing water retention and also helps in enhancing the bulkiness of stool by increasing stool mass, as a result makes the defecation process easier
- Proper intake of fibre is also associated with improving colonic motility and also helps to promote the health of colonic wall thus its consumption is thought to be very effective for accelerating the healing process
- Apart from that fibre plays vital role in reducing the pressure in the colon as well thus helps to avert flare-ups of diverculitis
- It is better to consume 15 to 20 g of crude fibre daily whereas soluble fibre should be consumed about 30 to 60 g per day
- Diet should contain whole grain cereals, wheat bran, brown rice, green leafy vegetables, nuts, fruits, oat meal, legumes and beans as they all are high fibrous food

Proteins
- It is better to consume 1 g protein per kg of ideal body weight daily
- Diet should contain both plant and animal proteins and it is better to consume all essential amino acids through diet for obtaining optimum nutritional status
- Among all amino acids, glutamine is considered as one of the most important amino acids required for preventing diverticular disease as glutamine helps in strengthening the colonic wall and also helps to protect the colonic wall from further damages
- Cabbage, spinach, dairy products, chicken, tofu, beans, lentils, fish are good sources of glutamine thus they should be included in the diet in order to promote early recovery
Fats

- Fat consumption should be restricted as too much fat can worsen the condition
- Fat should not be consumed more than 30g per day and it is better to consume fat from plant sources like plant seed oil, nuts, nut butter etc as they contain unsaturated fatty acids, which are extremely beneficial for health
- Consumption of omega 3 fatty acid is also very beneficial for patients with diverticular disease as they help in fighting against inflammation and also help in decreasing the prevalence of colon cancer
- It should be kept in mind that for fulfilling the requirement of fat in body, one should consume unsaturated fatty acid whereas consumption of saturated fat and Trans fat should be strictly avoided
Vitamins and Minerals
- All vitamins and minerals should be consumed as per RDA but special consideration should be provided on fat soluble vitamins (as fat consumption get reduced) and iron
- It is better to focus on iron consumption because there is a risk of developing anemia due to rectal bleeding
Water
- About 8 glasses of water should be consumed daily
- It helps to make the stool soft and also helps in clearing the bowel thus helps to provide relief to the patients
Foods that should be excluded from the diet

Below listed foods should be excluded from the diet of an individual with diverticular disease –
- Red meat
- Fried foods
- Processed foods
- Full fat dairy products like ice cream, butter milk etc
- Greasy foods
- Smoothies
- Soda
General dietary consideration
- It is better to consume high fibre diet whereas during flare ups of diverticulitis, it is better to consume a clear fluid diet such as clear apple juice or grape juice or cranberry juice or popsicles or broth etc while the intestine heals
- Regular exercise is mandatory as physical activity helps in increasing bowel movement, which subsequently prevents constipation
- It is better to maintain a healthy body weight
- Better to say no to alcohol and cigarettes
Source:
Carabotti, M., Annibale, B., Severi, C. and Lahner, E., 2017. Role of fiber in symptomatic uncomplicated diverticular disease: a systematic review. Nutrients, 9(2), p.161.
Floch, M.H. and White, J.A., 2006. Management of diverticular disease is changing. World Journal of Gastroenterology: WJG, 12(20), p.3225.
Lanas, A., Abad-Baroja, D. and Lanas-Gimeno, A., 2018. Progress and challenges in the management of diverticular disease: which treatment?. Therapeutic advances in gastroenterology, 11, p.1756284818789055.
Puyuelo, C.J.G., Sopeña, F. and Arbeloa, A.L., 2015. Colonic diverticular disease. Treatment and prevention. Gastroenterologia y hepatologia, 38(10), pp.590-599.
Tarleton, S. and DiBaise, J.K., 2011. Low‐residue diet in diverticular disease: putting an end to a myth. Nutrition in Clinical Practice, 26(2), pp.137-142.
Ünlü, C., Daniels, L., Vrouenraets, B.C. and Boermeester, M.A., 2012. A systematic review of high-fibre dietary therapy in diverticular disease. International journal of colorectal disease, 27(4), pp.419-427.