What is peptic ulcer disease?
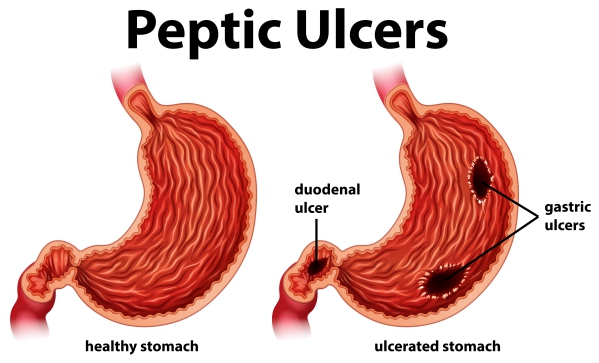
Peptic ulcers are sores that occurs in the lining of the stomach, duodenum, which is the first part of the small intestine starting just after the stomach, and the oesophagus. The most common causes of peptic ulcer disease (PUD) are Helicobacter pylori (H. pylori) infection and long-term use of Non-Steroidal Anti-Inflammatory Drugs (NSAIDs), resulting in inflammation of the stomach wall.
Pain or burning sensation in the upper abdomen that occurs after meals is the most common symptom. However, the majority of people with PUD does not experience any symptom.
In the United States alone, around 5 million citizens are affected by PUD annually. People above the age of 45 years are more frequently affected.
What are the causes and risk factors of peptic ulcer disease?
The stomach’s inner surface is covered with a mucus layer that protects it from stomach acid. A decrease in the mucus layer thickness or an increase in secretion of acid will result in inflammation of the stomach wall, leading to a painful sore. Common causes of peptic ulcer disease include:
- Helicobacter pylori infection (90%): this is a bacterium that lives in the mucus layer of the stomach. The latter can increase the amount of acid being secreted, breaks down the mucus protective layer and causes inflammation of the stomach wall.
- Long-term use of certain medications: aspirin and NSAIDs decrease the effectiveness of the mucus protective layer, making you more susceptible to peptic ulcer disease. In addition, other medications like steroids, selective serotonin reuptake inhibitors and anticoagulants can also cause PUD.

There are certain factors that can increase your risk of developing PUD such as cigarette smoking, alcohol consumption, excessive stress and spicy foods.
What are the signs and symptoms of peptic ulcer disease?
Around 70% of people with peptic ulcer disease experience no symptoms. However, later on, these people may suffer from ulcer-related complications such as haemorrhage and stomach perforation. On the other hand, symptomatic people may complain of:
- Upper abdominal pain: 80% of people with PUD will experience this and it is usually a burning sensation that occurs after meals.
- Abdominal fullness and bloating
- Nausea
- Early satiety
People with severe PUD may complain of:
- Unexplained weight loss
- Black stool
- Vomiting of blood (Coffee-ground vomitus)
- Loss of appetite
- Severe nausea
- Sudden, severe and diffuse abdominal pain which occurs due to the perforation of the stomach wall

Making a diagnosis
Your doctor will take a good and detailed history from you in order to know more about your symptoms and risk factors. PUD is usually suspected when you have a history of burning abdominal pain, long-term use of NSAIDs or a previous history of H. pylori infection. This is followed by a physical examination during which your doctor will look for signs of PUD and rule out other medical conditions.
The best diagnostic test for PUD is upper endoscopy to directly visualise the ulcer. In this procedure, a tube with a camera is inserted through your mouth up to your stomach. In addition, in case your doctor suspects H. pylori infection or stomach cancer, he/she may take some samples during the upper endoscopy to be analysed in the laboratory. The suspicion of stomach cancer is based on alarm signs and symptoms such as anaemia, unintentional weight loss, stomach bleeding and difficulty swallowing.
Furthermore, your doctor may order a complete blood count to look for anaemia which may be due to recurrent stomach bleeding.
If your doctor suspects H. pylori infection and upper endoscopy could not be performed, he/she may order a urea breath test to test for the presence of H. pylori.
In case of severe abdominal pain and rigidity, your doctor may order a plain abdominal x-ray to rule out perforation of the stomach.

What is the treatment of peptic ulcer disease?
The treatment of PUD depends on the underlying cause:
- H. pylori positive PUD: In this case, your doctor will prescribe a Proton Pump Inhibitor (PPI) such as omeprazole and 2 antibiotics, usually clarithromycin and amoxicillin. The PPI works by decreasing the gastric acid secretion to help improve your symptoms.
- Medication-induced PUD: If your doctor suspects that your symptoms are being caused due to any medications such as NSAIDs or aspirin, he/she will advise you to discontinue the offending medications and use a PPI. However, if ever you really need to continue the use of the medications, then your doctor will advise you to take a PPI along with the medications.
Some other medications can be prescribed by your doctor to relieve your symptoms such as antacids, H2-receptor blockers (cimetidine and ranitidine) or cytoprotective agents (misoprostol and sucralfate). These medications help to enhance mucus production and prevent gastric acid over-secretion.
If a pregnant woman is suffering from PUD, the focus of the treatment is usually acid suppression using a PPI. However, if H. pylori is present, antibiotics are deferred until delivery.
Complications of peptic ulcer disease
If PUD is left untreated, serious complications may arise, these include:
- Perforation of the stomach wall: this result in an abrupt and very severe abdominal pain and the abdomen will be board-like hard.
- Obstruction of the stomach: as a result of the inflammation caused by PUD, the normal stomach layer will be replaced by scar tissue which may obstruct the opening of the stomach. This may manifest as early satiety, vomiting and loss of weight.
- Gastric cancer: people with H. pylori positive PUD are at increased risk of developing gastric cancer.
- Internal bleeding: this may manifest as bloody or coffee-ground vomiting, black stool or signs of anaemia.

Prevention of peptic ulcer disease
There are several ways to prevent the development of PUD, these include:
- Cigarette smoking cessation
- Avoidance of alcohol
- Minimize intake of spicy foods
- Avoidance of offending drugs such as aspirin and NSAIDs
- If use of offending drugs are necessary, a PPI and intake of the drugs after meals are advised
- Good hand hygiene to reduce the risk of getting infected by H. pylori
Prognosis
Addressing the underlying cause of PUD results in excellent prognosis, provided that the treatment plan is followed with care. However, there is a 10-20% risk of recurrence.

Source:
J. Alastair, I. and Simon, M., 2016. Davidson’s Essentials of Medicine. 2nd ed. London: ELSEVIER.
Parveen, K. and Michael, C., 2017. Kumar & Clarks Clinical Medicine. 9th ed. The Netherlands: ELSEVIER.
Anand, BS., 2020. Peptic Ulcer Disease
Lanas A, Chan FKL. Peptic ulcer disease. Lancet. 2017 Aug 5. 390 (10094):613-24.


