What is Ulcerative Colitis?
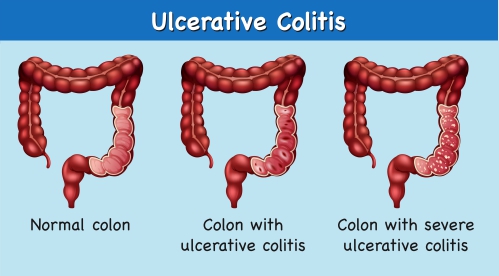
Ulcerative colitis is one of the two major types of inflammatory bowel disease, along with Crohn’s disease. This condition affects mainly the large intestines unlike Crohn’s disease which can affect any part of the digestive tract (gastrointestinal tract). The gastrointestinal tract includes the mouth, esophagus, stomach, small intestines, large intestines (colon) and rectum. In ulcerative colitis, the inner layer of the large intestines is affected and it characteristically starts affecting the rectum and progresses to the large intestines. This condition causes inflammation and sores (ulcers) in your digestive tract resulting in signs and symptoms such as rectal bleeding, diarrhoea, abdominal pain and fever.
In the United States, around 1 million people are affected by ulcerative colitis. This disease is three times more common than Crohn’s disease. In addition, it is more common in whites than blacks or Hispanics. However, it is 2-4 times more common in Ashkenazi Jews. Women are more commonly affected by the disease than men. Ulcerative colitis can affect people of all ages but is more common in people aged between 15-25 years and 55-65 years.
What are the causes and risk factors of ulcerative colitis?
The exact cause of ulcerative colitis is not known but certain factors have been associated with the disease and these include:
- Family history: Having a parent or sibling affected by ulcerative colitis, increases your risk of developing the disease.
- Immune reactions: If a virus or bacterium invades your gastrointestinal tract, your immune system will release antibodies in an attempt to fight these organisms. However, this results in inflammation which may contribute to the development of ulcerative colitis.
- Race: Whites are more commonly affected by the disease than blacks and Hispanics. In addition, it is more common in Ashkenazi Jews.
- Age: Ulcerative colitis is more common in people aged between 15-25 years and 55-65 years.
- Sex: Women are more commonly affected by the disease than men.
- Non-steroidal anti-inflammatory drugs (NSAIDs) use: The use of NSAIDs is to be avoided in people suffering from ulcerative colitis as it may make your symptoms worse.
- Stress: Psychological and psychosocial stress factors can aggravate your symptoms.
- Cigarette smoking: Cigarette smoking has shown to be a protective factor for ulcerative colitis.
- Milk consumption: Milk consumption may make your symptoms worse.

What are the sign and symptoms of ulcerative colitis?
The signs and symptoms of ulcerative colitis include:
- Rectal bleeding
- Diarrhoea with pus or blood
- Mucous discharge from the rectum
- Tenesmus: a feeling of the need to have a bowel movement, with little or no stool passed.
- Lower abdominal pain and cramping
- Severe dehydration
- Rectal pain
- Weight loss
- Fever
- Excessive fatigue
- Inability to gain weight and grow in children

There are some signs and symptoms which may arise outside of the colon and these include:
- Inflammation of the eye (uveitis).
- Tender red nodules or lumps that are usually located on both shins (erythema nodosum).
- Painful pustules or nodules that progressively become ulcers (pyoderma gangrenosum).
- Inflammation of the membranes surrounding your lungs which result in sharp chest pain upon breathing (pleuritis).
- Pain and stiffness in your spine (ankylosing spondylitis)
Making a diagnosis
To make a diagnosis, your doctor will first take a detailed history from you to know more about your symptoms. After the history taking, your doctor will perform a thorough physical examination to look for signs of ulcerative colitis. Your doctor may order some test to confirm the diagnosis and these include:
- Serologic markers: These are antibodies that are specific to the disease and these include Antineutrophil cytoplasmic antibodies (ANCA) and anti-Saccharomyces cerevisiae antibodies (ASCA). ANCA is more commonly associated with ulcerative colitis. A positive ANCA test suggests ulcerative colitis and a negative test suggests Crohn’s disease.
- Complete Blood Count (CBC): The CBC is done to check for anaemia and an increased platelet count.
- Metabolic panel: Findings on the metabolic panel may include decreased protein level (hypoalbuminemia), decreased potassium level (hypokalemia), decreased magnesium level (hypomagnesemia), elevated alkaline phosphatase (this indicates the presence of primary sclerosing cholangitis which is a disease affecting the liver).
- Erythrocyte sedimentation rate (ESR): ESR is an inflammatory marker which is usually elevated in ulcerative colitis.
- C-reactive protein level: This test correlate with the disease activity and is also an inflammatory marker.
- Stool studies: Stool studies are done to rule out infectious processes within the colon. In addition, it is also done to check for blood in stool.
- Colonoscopy and biopsy: Colonoscopy is a procedure during which your doctor inserts a tube containing a camera at its end into your rectum to have direct visualisation of the inside of your colon. At the same time, a sample of your colon may be taken to be analysed under the microscope to confirm the diagnosis of ulcerative colitis.
- Radiologic assessment: Ultrasonography, Computed Tomography (CT) scan and Magnetic Resonance Imaging (MRI) scan is useful to determine the effects of the disease on your bowel. In addition, an abdominal x-ray may be done to rule serious complications like a perforated bowel.

What are the treatments of ulcerative colitis?
The treatments of ulcerative colitis include:
- Anti-inflammatory drugs: These drugs are often the first step in the management of ulcerative colitis. 5-aminosalicylates is a type of inflammatory drugs used to treat ulcerative colitis and examples include sulfasalazine, mesalamine and olsalazine amongst others. In addition, corticosteroids can also be used to decrease the inflammatory processes involved in ulcerative colitis and these include prednisolone and budesonide. Corticosteroids are often associated with several side-effects, which is why they are given for a short period of time only.
- Immunosuppressors: This class of drug works by suppressing your immune system to reduce inflammation. Examples include azathioprine, cyclosporine and tofacitinib.
- Biologics: This class of drug works by targeting the proteins made by your immune system and examples include infliximab and vedolizumab amongst others. Infliximab is also known as tumour necrosis factor (TNF) inhibitors. TNF is a protein made by your immune system.
- Antidiarrheal medications: These drugs are used to treat severe diarrhoea and an example include loperamide.
- Pain killers: These drugs are used to relieve the pain associated with ulcerative colitis.
- Iron supplements: Iron supplements are given to treat the anaemia associated with ulcerative colitis.
- Surgery: Surgery is considered as the definitive way to treat ulcerative colitis. It is often indicated when there is failure of medical management or controlled bleeding within the colon. During this procedure, part of the colon is removed and the remaining colon is stitched back together. Unfortunately, if the entire colon along with your rectum is removed, a bag to collect your stool will be installed.

What are the complications of ulcerative colitis?
If ulcerative colitis is left untreated, the following complications may ensue:
- Severe intestinal bleeding
- Perforated colon
- Osteoporosis (bone loss)
- Severe dehydration
- Inflammation of your eyes, joints and skin
- Toxic megacolon- this is when your colon swells rapidly which can be life-threatening.

Prognosis
Ulcerative colitis is a disease which can negatively affect your quality of life. However, seeking medical advice early and following your treatment plan properly and seriously can help to reduce your symptoms and improve your quality of life.
Source:
J. Alastair, I. and Simon, M., 2016. Davidson's Essentials of Medicine. 2nd ed. London: ELSEVIER.
Parveen, K. and Michael, C., 2017. Kumar & Clarks Clinical Medicine. 9th ed. The Netherlands: ELSEVIER.
Medscape. 2020. Ulcerative Colitis.
Medscape. 2020. Ulcerative Colitis Workup.
Medscape. 2020. Ulcerative Colitis Treatment & Management.