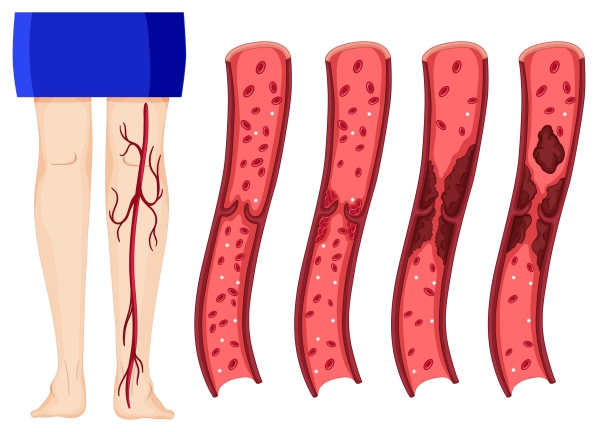
What is Deep Vein Thrombosis?
Deep vein thrombosis is when a blood clot (also known as a thrombus) forms in a deep vein, most commonly in your lower extremities. This is a serious condition that can lead to more severe complications which can be even life threatening. The clot causes symptoms at the level of its formation, but can also be dislodged and travel through your circulatory system and gets stuck in your pulmonary artery. This condition is called pulmonary embolism. Around 300,000 people die from massive pulmonary embolism per year in the United States.
The major causes of deep venous thrombosis are mainly immobility and hypercoagulability. Unlike thrombus formation in arteries, venous thrombosis can occur in healthy veins. Even if there are several factors that can put you more at risk of having a deep vein thrombosis, it is preventable in many cases.
Causes and Risk factors
You are at increased risk of having deep vein thrombosis if you are not able to move properly for example following an injury or major surgery. It can also arise if you take certain medications or have any medical conditions interfering with your blood circulation or clotting. The known causes and risk factors are listed below:
- Immobilization: This can be following a major injury or surgery which is causing immobilization or made you bedridden. It can also be due to a prolonged airplane flight in which you have limited movement. Medical conditions such as heart failure, stroke, cancer, obesity or other neurological disorders can all contribute to stasis of blood in your limbs due to insufficient limb movement.
- Age: Deep vein thrombosis become more common with increasing age. This may be related to the increased risk of having other medical problems which can put you more at risk of having a deep vein thrombosis. However, deep vein thrombosis can occur at any age.
- Prior history of Deep vein thrombosis: If you had deep vein thrombosis in the past, you are predisposed to develop it again in the future.
- Pregnancy: When you are pregnant, you are said to be in a hypercoagulable state. This means that your blood has a higher tendency to clot.
- Smoking: Smoking makes your blood thicker. This alters the way blood flows in your blood vessels. Besides, it also affects blood clotting, thus, promoting the formation of thrombus.
- Genetics: Certain genetic defects can also lead to a hypercoagulable state.
- Drugs: Certain drugs can increase your risk of having deep vein thrombosis. These include: oral contraceptives, hormonal replacement therapies, tamoxifen, glucocorticoids and antidepressants.

Signs and symptoms
In many cases, people have a thrombus in their lower limbs and are not even aware as no symptoms may be present. Furthermore, the symptoms present in deep vein thrombosis can occur in many other conditions. Deep vein thrombosis is suspected in anyone with the following:
- Swelling of limb
- Painful limb
- Warmth over painful area
- Redness over the limb
- Change of skin colour over the warm or tender area

Most of the time, people with deep vein thrombosis present at the emergency department when it has progressed to a pulmonary embolism. This is a life threatening condition which can present with the signs and symptoms below:
- Sudden onset of shortness of breath
- Chest pain which gets worse upon breathing
- Rapid pulse
- Coughing up blood
- Dizziness
- Decreased blood pressure
- Skin turning blue
Making a diagnosis
After taking a good history and performing a thorough physical examination, your doctor may already know if you have deep vein thrombosis. Depending on all the information obtained by your doctor, he/she may classify whether you are at low, moderate or high risk of having a thrombus. However, to confirm the diagnosis, your doctor may perform some furthers tests. These include:
- D-dimer levels: D-dimer is a substance that is released when a clot is broken down. If it is present in high levels in your blood, you are more likely to have deep vein thrombosis.
- Ultrasound: This is commonly used to locate the presence of a thrombus in the veins running along your limbs. This procedure uses sound waves to recreate the structures being visualized.
- Venography: In this procedure, a dye is injected in a large vein in your lower limbs and an X-ray is taken to see if there is anything obstructing the flow of the dye. This will give an idea whether there is a thrombus along the vein.

Treatment of Deep vein thrombosis
It is very important to manage deep vein thrombosis early as it can anytime progress to a pulmonary embolism. The aim is to prevent the clot from getting bigger and prevent it from getting dislodged.
Treatment of deep vein thrombosis include:
- Anticoagulants: These drugs, also known as blood thinners, decrease the tendency for your blood to clot. It also stop the progression of the blood clot and makes it less likely for you to have more clots. Some examples include: heparin, enoxaparin, warfarin or fondaparinux. You will have to get your blood checked regularly and your doctor will adapt your treatment accordingly.
- Thrombolytic drugs: These drugs work by breaking down clots. These are given directly in your veins and are mostly used in severe cases.
- Vein filter: If the above fail or cannot be prescribed in certain cases, filters can be inserted in your major vein called the inferior vena cava to prevent the dislodged blood clot to enter the heart and travel to the lungs.
- Compression stockings: These are used as a means to prevent stasis of your blood in your lower limbs. This will prevent the formation of blood clots in your veins.
- Surgery: Surgical removal of the clots can be done as an alternative. This can be carried out with the help of a catheter.

Complications
The main and life threatening complication of deep vein thrombosis is pulmonary embolism. This can lead to irreversible damage to your lungs. It is very important to recognise the signs and symptoms of a pulmonary embolism and seek medical help immediately.
Other complications may include skin ulcerations, recurring deep vein thrombosis and damage and scarring of your veins.
Prevention
Several measures can be taken to decrease your risk of developing deep vein thrombosis, namely:
- Try to get moving as soon as possible after an injury or surgery depending on what your doctor recommends you and as tolerated. Avoid long periods of travel where you sit still. If you do so by car, try to stop frequently to walk for at least a few minutes.
- Stop smoking
- Maintain a healthy weight
- Exercise regularly
- Wear compression stockings if you are at a higher risk of having deep vein thrombosis
Source:
J. Alastair, I. and Simon, M., 2016. Davidson’s Essentials of Medicine. 2nd ed. London: ELSEVIER.
Parveen, K. and Michael, C., 2017. Kumar & Clarks Clinical Medicine. 9th ed. The Netherlands: ELSEVIER.
Oxford handbook of Clinical medicine, 10th edition
Patel, K., 2019. Deep Venous Thrombosis (DVT)



