What is diabetic retinopathy?
Diabetic retinopathy is a complication affecting the eyes that arises due to uncontrolled and longstanding diabetes. The retina is a light-sensitive tissue located at the back of the eye. In diabetic retinopathy this tissue is damaged resulting in vision problems.
In the United States, diabetic retinopathy is the leading cause of new blindness in people aged between 25-74 years. Around 700,000 Americans are affected by this disease.
What are the causes of diabetic retinopathy?
Uncontrolled and longstanding diabetes may affect your eyes leading to diabetic retinopathy. This can happen via several mechanisms:
- Platelets and blood thickness (viscosity): Diabetes causes your red blood cells and platelets to stick to each other which results in obstruction of your small blood vessels found in your retina. This leads to retinal ischaemia- this is when the blood supply to your retina is diminished resulting in a shortage of oxygen leading to damage or dysfunction of the tissue.
- Retinal haemorrhage: Elevated blood glucose levels due to diabetes weakens the walls of your retinal blood vessels. As result, tiny bulges (microaneurysms) arises in the blood vessel walls which may burst, leading to haemorrhages. These haemorrhage may be seen during an eye examination as flame-shaped haemorrhages or as blot and dot haemorrhages.
- Macular edema: The area at the centre of the retina is known as the macula. This portion of the retina allows you to read, recognize faces, colours and see objects with great detail. Macular edema occurs when there is build-up of fluid in the macula which causes the macula to swell and thickens, distorting your vision.
- Hypoxia: As your retinal blood vessels are getting more damaged, eventually it is blocked completely preventing any oxygen to reach your retina. Ischaemia is when there is a reduction of blood supply which eventually leads to hypoxia which is reduction of oxygen supply. These result in proliferation or development of new blood vessels in an attempt to compensate for the lack of oxygen which is known as neovascularisation. This process further decreases your vision and makes you more prone to retinal haemorrhages.

What are the risk factors of diabetic retinopathy?
There are several factors which make increase your risk of developing diabetic retinopathy and these include:
- Duration of diabetes: 75-95% of diabetic people develop diabetic retinopathy after 15 years. In addition, if your diabetes is not controlled properly, it may lead to diabetic retinopathy even sooner.
- Hypertension: Hypertension increases your risk of developing diabetic retinopathy in diabetic people.
- Hypercholesterolemia: Elevated cholesterol level may cause further damage to your retina as it causes fluids to escape your blood vessels leading to hard exudates on the retina.
- Pregnancy: Pregnancy in a diabetic women may increase the risk of developing diabetic retinopathy.
What are the signs and symptoms of diabetic retinopathy?
Initial stages of the disease may be asymptomatic. However, as the disease progresses, you may experience symptoms like:

- Blurred vision
- Floaters: this is when you see tiny shadows in your vision.
- Distorted vision
- Dark areas in your vision
- Loss of vision
- Impaired colour vision
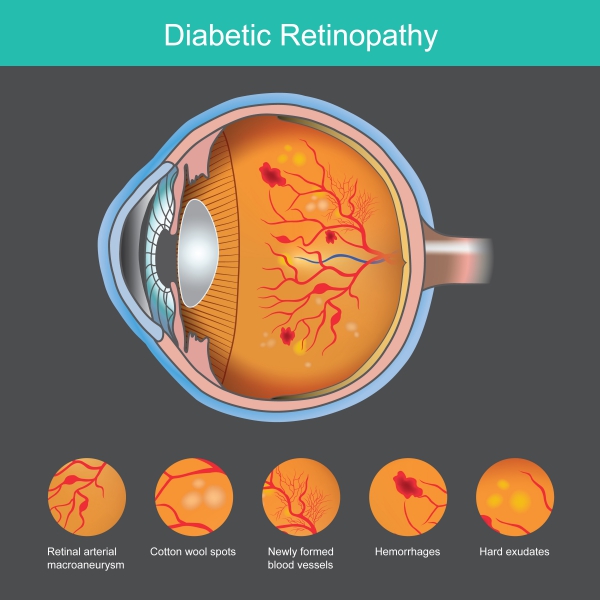
Upon examination of your eyes, your doctor may see signs of diabetic retinopathy which include:
- Flame-shaped haemorrhage: this occurs when the microaneurysms rupture in the superficial layer of your retina.
- Bot and blot haemorrhage: this occurs when the microaneurysms rupture in deeper layers of your retina.
- Macular edema and hard exudates: when the retinal blood vessel walls are damaged, it allows the leakage of blood proteins and fats which results in macular edema and hard exudates. Macular edema is the leading cause of vision problem in diabetic people.
- Cotton-wool spots: when there is no blood supply to some parts of the retina, it results in the death of the nerves which can be seen as fluffy white patches on the retina.
There are some other disease which may resemble diabetic retinopathy and these include:
- Central retinal vein occlusion
- Branch retinal vein occlusion
- Retinal macroaneurysm
- Sickle cell disease
- Valsalva retinopathy
- Macular edema

Making a diagnosis
To make a diagnosis, your doctor will first take a detailed history from you to know more about your symptoms. After the history taking, your doctor will perform an eye examination to look for signs of diabetic retinopathy. He/she will use an apparatus known as a fundoscope which will allow visualisation of the interior structures of your eye. Your doctor may use some drops to dilate your pupils if necessary for the examination. To confirm the diagnosis, your doctor may order some tests and these include:
- Fasting glucose and haemoglobin A1c (HbA1c): These tests are essential to diagnose diabetes and to determine if your diabetes is controlled or not. The risk of developing diabetic retinopathy at 10 years is more if your HbA1c is greater than 6% and your fasting plasma glucose levels is more than 108 mg/dl.
- Fluorescein angiography: This is a procedure during which a dye in injected into your bloodstream while your doctor examines your eye. Photographs are taken to assess the blood flow in your retinal blood vessels.
- Optical Coherence Tomography (OCT): OCT uses light to assess the thickness and presence of swelling within your retina. This test is particularly useful in the diagnosis of diabetic macular edema.
- B-scan ultrasonography: if the retina cannot be visualised properly due to another disease, then this test can be used to assess your retina.

What are the treatments of diabetic retinopathy?
There are several treatment options for the management of diabetic retinopathy and these include:
- Glucose control: Keeping the HbA1c level below 7% prevents or at least minimizes the long-term complications of diabetes mellitus, including diabetic retinopathy.
- Ovine hyaluronidase therapy: Injection of ovine hyaluronidase into the eye is safe and efficient to clear haemorrhages located at the back of the eye.
- Vascular Endothelial Growth Factor (VEGF) inhibitors: These drugs have proved to improve your vision and were more efficient than laser photocoagulation. These drugs work by preventing the growth of new blood vessels and therefore improving your vision.
- Laser photocoagulation: This treatment option uses high-focused beam of light energy to coagulate parts of the retina and is particularly useful in the setting of macular edema
- Regular physical exercise: This will help to better control your diabetes as exercise makes your body absorb more glucose and maintain a healthy weight thereby reducing the complications of diabetes and diabetic retinopathy.
- Panretinal photocoagulation: This treatment is preferred in the case of proliferative diabetic retinopathy. The laser is applied over the whole retinal surface, sparing the central macular area, to prevent development of new blood vessels (neovascularisation).
- Vitrectomy: Vitrectomy is a surgical procedure during which your eye doctor removes the gel-like fluid located at the back of the eye to have better visualisation of the retina and be able to do repairs. It is particularly useful in removing blood present at the back of the eye that prevents your doctor to assess your retina.
- Cryotherapy: If laser photocoagulation is not possible due to cataract or haemorrhages, cryotherapy may be applied instead. This technique uses a very cold metal probe to create an adhesive scar that seals the retina against the wall of the eye.

What are the complications of diabetic retinopathy?
If diabetic retinopathy is left untreated, several complications may ensure and these include:
- Retinal detachment: When neovascularisation occurs, it may create some scar tissue on the retina which causes it to be pulled away from the back of the eye. This results in floaters, flashes of light or even severe vision loss.
- Vitreous haemorrhage: This is when there is bleeding in the gel-like fluid found at the back of the eye which results in some dark spots if the bleeding is mild but if sever, completely visual loss may occur.
- Glaucoma: The new blood vessels being formed can block the front part of the eye, preventing it from removing excess fluid from the eye. This results in an increase in pressure within the eye which is also known as glaucoma. Eventually, glaucoma may damage the optic nerve which is responsible to bring images to your brain. If glaucoma is left untreated, it can lead to permanent visual loss.
Prognosis
Unfortunately, around 8000 eyes become blind every year due to diabetes. However, early treatment of diabetic retinopathy using panretinal photocoagulation reduces the risk of severe visual loss by 50%.


Source:
J. Alastair, I. and Simon, M., 2016. Davidson's Essentials of Medicine. 2nd ed. London: ELSEVIER.
Parveen, K. and Michael, C., 2017. Kumar & Clarks Clinical Medicine. 9th ed. The Netherlands: ELSEVIER.
Bhavsar, A., 2020. Diabetic Retinopathy Treatment & Management: Approach Considerations, Glucose Control, Aspirin Therapy









