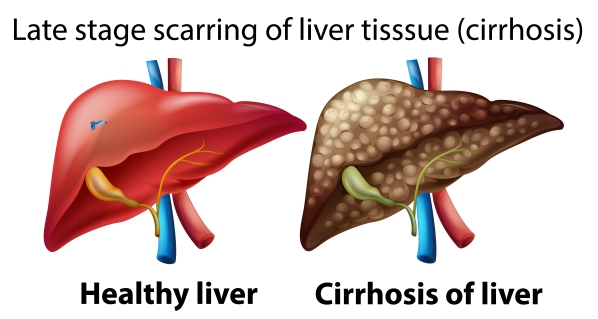
What is liver cirrhosis?
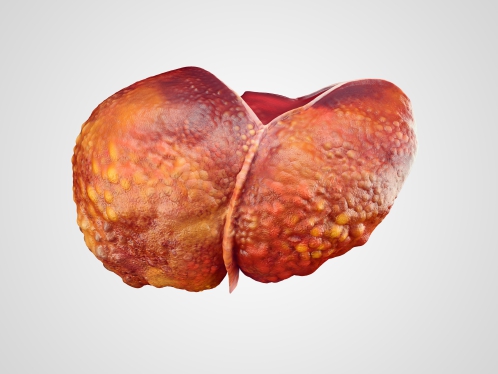
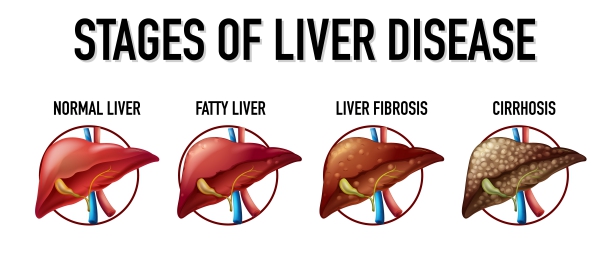
Cirrhosis of the liver is the severe scarring of the liver due to diseases such as hepatitis and alcoholic liver disease. When there is injury to the liver, it will try to repair itself, thus forming scar tissue. The liver is located in the upper right side of your abdomen beneath the ribs. It is responsible for the production of bile which is necessary for the absorption of vitamins A, D, E and K. In addition, it also produces clotting proteins and glucose. Furthermore, the liver helps in removing toxic substances from your blood.
Liver cirrhosis is the ninth leading cause of death in the United States. As scarring of the liver progresses, the liver’s ability to perform its functions decrease and becomes a life-threatening condition. The damage done to the liver is often irreversible. However, early diagnosis can stop or slow down the progression of the disease.
What are the causes of liver cirrhosis?
There are several factors and diseases which can result in liver cirrhosis, such as:
- Chronic viral infection of the liver- hepatitis B, C and D.
- Non-alcoholic liver disease- fat accumulation in the liver.
- Alcoholic liver disease.
- Hemochromatosis- iron accumulation in the body.
- Cystic fibrosis- a hereditary disease affecting the lungs and digestive system.
- Wilson’s disease- copper accumulation in the liver.
- Biliary atresia- in this condition the bile ducts are scarred and blocked.
- Hereditary sugar metabolism disorders.
- Alpha-1 antitrypsin deficiency- a hereditary disease that affects the lungs and liver.
- Autoimmune hepatitis- this is when your own immune system attacks your liver cells.
- Primary sclerosing cholangitis- this is when scarring of the bile ducts develops.
- Syphilis.
- Drugs- methotrexate, isoniazid, acetaminophen and antidepressants.
- Being overweight or obese.

What are the signs and symptoms of liver cirrhosis?
The signs and symptoms of liver cirrhosis may not be apparent during early stages of the disease. However, as the disease progresses, the following signs and symptoms may arise:
- Feeling very sick, tired and weak.
- Loss of appetite.
- Jaundice- yellowing of the skin and white part of the eyes.
- Unintentional loss of weight.
- Loss of sexual desire (libido).
- Darkening of urine.
- Pale stools.
- Easy bruising and bleeding.
- Peripheral oedema- swelling of the legs.
- Ascites- abdominal distention due to fluid accumulation.
- Nose bleed.
- Gynaecomastia- when males develop breast tissue.
- Irregular menstrual period not related to menopause.
- Confusion and drowsiness.

Making a diagnosis
To make a diagnosis, your doctor will first take a detailed history from your to know more about your symptoms. After the history taking, he/she will carry out a thorough physical examination to look for signs of liver cirrhosis, such as:
- Hand tremors
- Jaundice
- Reddened palms and face
- Enlargement of the liver or spleen
- Gynaecomastia
- Confusion
Several tests can be done to confirm the diagnosis of liver cirrhosis, such as:
- Blood tests: complete blood count, coagulation blood tests, serum albumin, liver functions tests and alpha fetoprotein.
- Ultrasound scan of the liver: this is to identify any mass or abnormality within the liver.
- Endoscopy: This is to look for oesophageal varices which occur as a result of portal hypertension due to scarring of the liver.
- Magnetic Resonance Imaging (MRI) and Computed Tomography (CT) scan: this is to acquire more detailed information about the structure of the liver.
- Liver biopsy: In this procedure, your doctor take a small piece of your liver, using a needle to send to the laboratory for analysis.

What are the treatments for liver cirrhosis?
The treatment of cirrhosis depends on the underlying causes and the severity of liver damage. The goals of the management are to slow down progression, improve symptoms and prevent complications from the disease. The management of liver cirrhosis include:
- Drugs to manage hepatitis and primary biliary cirrhosis.
- Weight loss.
- Eating a balanced diet.
- Reducing salt intake.
- Alcohol avoidance: stopping the use of alcohol can significantly improve your health. However, if you are addicted to alcohol, your doctor will recommend you enrolling for a treatment program for alcohol addiction.
- Smoking cessation.
- Doing regular physical exercise.
- Beta-blockers: these drugs help to manage portal hypertension which can result in ascites and oesophageal varices. An example is metoprolol and its side effects include drowsiness, depression, dry mouth and tiredness.
- Diuretics: diuretics are used to remove excess water from the body. An example is furosemide.
- Antibiotics: these are given to treat infections which may occur due to ascites.
- Liver transplant surgery: this treatment strategy is considered in very advanced cases of liver cirrhosis, where the liver has stopped functioning completely. Liver transplant is a procedure during which your liver is replaced with a healthy liver from a deceased donor or with part of a liver from a living donor.

Complications of liver cirrhosis
If liver cirrhosis is left untreated, the following complications may develop:
- Portal hypertension: portal hypertension occurs when there is high blood pressure in the veins supplying the liver. This occurs because of the scarring of the liver which causes obstruction and hence increase the blood pressure in the veins. The portal vein brings blood from the intestines and spleen to the liver.
- Oedema: Portal hypertension and a decrease in the production of the protein albumin can lead to swelling of the legs (peripheral oedema) and abdomen (ascites).
- Splenomegaly: portal hypertension can eventually cause enlargement of the spleen which will result in decreased amount of white blood cells and platelets in your blood. This is usually the first sign of liver cirrhosis.
- Oesophageal and gastric varices: portal hypertension can result in excess pressure in the veins which will lead to oesophageal and gastric varices. These varices may burst to cause internal bleeding which can be life-threatening.
- Malnutrition: decreased function of the liver can result in decreased absorption of nutrients and eventually malnutrition.
- Infections: decreased white blood cells due to splenomegaly will make you more prone to infections.
- Hepatic encephalopathy: as the toxin-removal ability of the liver decreases, there will be an accumulation of toxins in your blood. These toxins affects the brain and leads to confusion and drowsiness.
- Increased liver cancer risk.
- Jaundice

Prevention of liver cirrhosis
There are several factors which may decrease your risk of developing liver cirrhosis, these include:
- Avoiding alcohol consumption.
- Maintaining a healthy weight.
- Adopting a healthy diet by including a lot of fruits and vegetables in your meals.
- Avoiding to share needles and having unprotected sex will decrease your risk of acquiring hepatitis B and C.
Prognosis
Alcohol cessation can significantly impact recovery from the disease. Among those with severe alcoholic cirrhosis, only 50% will survive for 2 years. As complications begin to arise, the recovery rate decreases. Liver transplant can help improving survival time. The earlier treatment is initiated, the better the prognosis.

Source:
Parveen, K. and Michael, C., 2017. Kumar & Clarks Clinical Medicine. 9th ed. The Netherlands: ELSEVIER.
Wolf, D., 2020. Cirrhosis.
NHS. 2020. Cirrhosis.