What is meningitis?
Meningitis is the inflammation of your meninges which are membranes that surround your brain. Meningitis can also be caused by infection of the fluids that surround the meninges.
Meningitis is most commonly caused by a viral or bacterial infection of the meninges. It affects people of all races. However in the United States, black people are more at risk than whites and Hispanic people.
Meningitis can resolve on its own after some weeks in certain cases but can also be life-threatening requiring emergency antibiotic treatment.
What are the causes of meningitis?
Viral infections of the meninges is the most common cause of meningitis in the United States. However, it can also be caused by drugs, bacterial, fungal and parasitic infections as well.
Bacterial meningitis occurs when bacteria enter the bloodstream to reach the brain and spinal cord. However, it can also occur when the bacteria directly infect the meninges especially after head surgery or trauma. The most common bacteria causing bacterial meningitis are Streptococcus pneumoniae, Neisseria meningitides, Listeria monocytogenes and Haemophilus influenza.
In the Unites States, most cases of viral meningitis are caused by enteroviruses- a group of viruses which are most common in early fall or late summer. Viral meningitis is often mild and resolves on its own. Other viruses which can cause viral meningitis include Human Immunodeficiency Virus (HIV), herpes simplex virus, mumps virus, West Nile virus, measles virus, rubella virus and rabies virus.

Fungal meningitis is rare in the United States and may resemble bacterial meningitis. People affected by Acquired Immunodeficiency Syndrome (AIDS) are predisposed to cryptococcal meningitis as their immune system are suppressed. It can be acquired by breathing in fungal spores that are usually found in bird droppings, soil and decaying wood. Fortunately, it is not spread from person to person. However, this disease can be a life-threatening condition if the appropriate treatment is not initiated early.
Parasitic meningitis can also be called eosinophilic meningitis. It is usually due to cysticercosis- a tapeworm infection in the brain. Amoebic meningitis is a life-threatening condition that is usually contracted through fresh water swimming. It is not spread from person to person but can be acquired by eating parasite-contaminated foods.
In addition, some drugs may also cause meningitis and these are Non-Steroidal Anti-Inflammatory Drugs (NSAIDs), metronidazole and intravenous immunoglobulin.
What are the risk factors for meningitis?
Risk factors for meningitis:
- Age: being less than 5 years old or more than 60 years old makes you more at risk of developing meningitis due to reduced functioning of your immune system.
- Diabetes mellitus.
- Adrenal insufficiency.
- Chronic kidney failure.
- Hypoparathyroidism.
- Cystic fibrosis.
- Immunosuppression: a suppressed immune system due to drugs, diseases or ageing predisposes you to opportunistic and bacterial infections.
- HIV infection: as HIV leads to AIDS, the reduced functioning of your immune system makes you more prone to opportunistic pathogens and streptococcus pneumoniae.
- Living in a community setting: living in military bases, boarding schools, dormitories or child care facilities increases your risk of developing meningitis.
- Splenectomy: removal of the spleen surgically makes you more prone to meningitis.
- Sickle cell disease.
- Alcoholism and liver cirrhosis.
- Sinusitis.
- Head trauma or surgery can facilitate contraction of meningitis.
- Thalassemia.
- Intravenous drug abuse.
- Bacterial endocarditis.
- Cancer.
- Incomplete vaccination schedules.

What the signs and symptoms of meningitis?
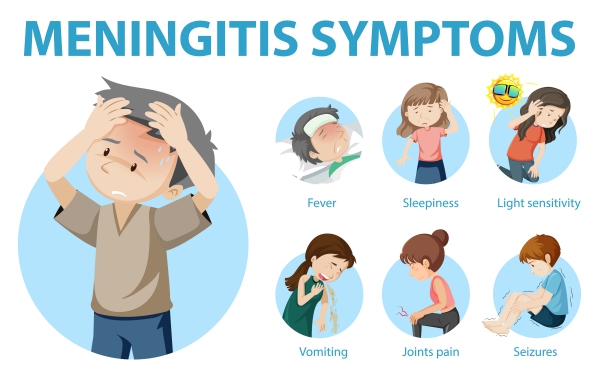
It is very difficult to differentiate between viral and bacterial meningitis based only on the signs and symptoms as they are very similar. Meningitis affects people of all ages, however, the signs and symptoms differs in newborns, infants and older people. As the condition can be life-threatening, identifying the signs and symptoms of meningitis is crucial.
Signs of meningitis in newborns and infants include:
- Inconsolable crying.
- High fever.
- Poor feeding.
- Irritability.
- Excessive sleepiness.
- Difficulty waking up from sleep.
- Vomiting.
- Bulging fontanel- a bulge in the soft part on top of the baby’s head.
- Neck stiffness.

Signs and symptoms in people above the age of 2 include:
- Severe headaches.
- Neck stiffness.
- High fever.
- Nausea and vomiting.
- Confusion.
- Seizures.
- Photophobia- discomfort when you look into bright lights.
- Loss of appetite.
- Skin rash- especially in meningococcal meningitis.
- Lethargy.
- Coma
Making a diagnosis
To make the diagnosis of meningitis, your doctor will first take a detailed history from you to know more about your symptoms. This is usually followed by a physical examination to look for signs of meningitis.
If the diagnosis of meningitis is suspected, a lumbar puncture should be performed as soon as possible. A lumbar puncture is a procedure during which your doctor inserts a needle in the space between your vertebrae to get assess to your cerebrospinal fluid- a fluid that surrounds your meninges and spinal cord. This fluid is then sent to the laboratory to determine if there is any infection and the type of meningitis. However, before the lumbar puncture, it is essential to carry out a computed tomography (CT) scan of the head to rule out high intracranial pressure (ICP)- if the lumbar puncture is performed while you have an elevated ICP, brain herniation can result which is deadly.

There are some blood investigations which can be performed such as serum electrolytes, serum glucose, blood urea nitrogen level, liver function test and HIV testing. If the diagnosis is uncertain, a blood culture can be done to direct the antibiotic therapy. In addition, serum procalcitonin is elevated in the case of bacterial meningitis.
What are the treatments for meningitis?
The treatment of meningitis depends on its cause. In the case of bacterial meningitis, antibiotics such as ampicillin, vancomycin and ceftriaxone can be used to fight off the infection. In addition, corticosteroids can be used to reduce inflammation of the brain and prevent complications.
Viral meningitis is usually benign and resolves on its own. However bed rest, drinking plenty of fluids and pain killers may help to ease your symptoms. Antivirals such as acyclovir can be used to help increase your rate of recovery.
Antifungals are used to fight off fungal meningitis.
What are the complications of meningitis?
If meningitis is left untreated, you can develop severe complications such as:
- Brain damage.
- Seizures.
- Hearing loss.
- Memory and learning disability.
- Kidney failure/
- Coma
- Death
- Difficulty in coordinating movement.
Prevention of meningitis
Several steps can be taken to prevent you from developing meningitis, these include:

- Washing your hands regularly.
- Maintaining your immune system up with a healthy diet containing plenty of fruits and vegetables.
- Making sure you have completed your vaccination schedules.
Prognosis
People with bacterial meningitis presenting with altered mental status, seizures and hypotension are at an elevated risk for complications and death. However, if meningitis is treated early, your risk of developing complications drops significantly.

Source:
J. Alastair, I. and Simon, M., 2016. Davidson's Essentials of Medicine. 2nd ed. London: ELSEVIER.
Parveen, K. and Michael, C., 2017. Kumar & Clarks Clinical Medicine. 9th ed. The Netherlands: ELSEVIER.
NHS. 2020. Meningitis.
Hasbun, R., 2020. Meningitis Workup.
Hasbun, R., 2020. Meningitis Clinical Presentation.
Hasbun, R., 2020. Meningitis Treatment & Management.