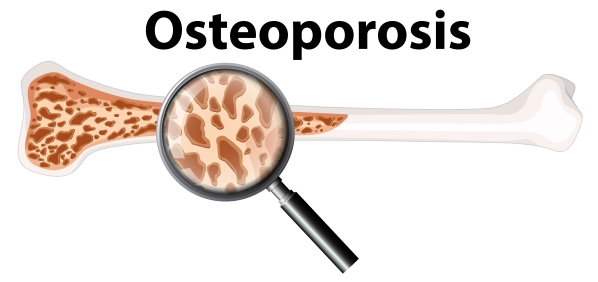
What is osteoporosis?
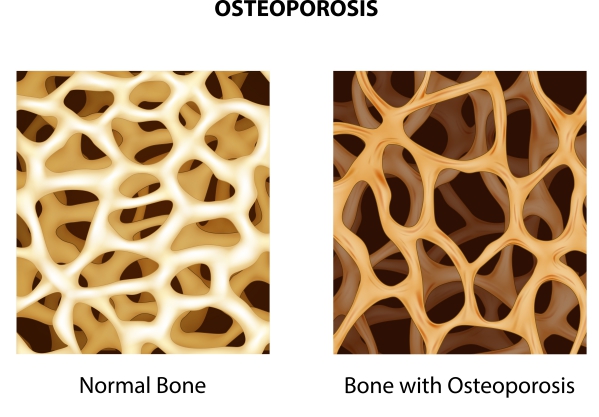
Osteoporosis is a disease which affects your bones, making them weak and brittle. Inside the bone, there are honeycomb-like spaces which are enlarged in osteoporosis. This causes the bone to lose density and strength. In addition, falls or even mild stresses such as coughing and bending over can result in fractures. The most common fractures due to osteoporosis involve the rib, hip, wrist and spine.
Bone remodelling is a lifelong process whereby new bone tissue is formed and mature bone tissue is removed from the bone. In osteoporosis, there is a disturbance in this process leading to more removal of mature bone tissue- also known as bone resorption- than creation of new bone tissue. This makes the bone fragile and vulnerable to fractures.
In the United States alone, more than 10 million people were affected by osteoporosis above the age of 50 and 43 million had low bone mineral density in the year 2010, according to the National Osteoporosis Foundation (NOF). Osteoporosis can affect everyone but it occurs more in Caucasians and Asians. In addition, post-menopausal women are at very high risk of developing the disease. However, there are medications, weight-bearing exercises and lifestyle modifications which can help to strengthen weak bones and prevent bone loss.
What are the causes and risk factors of osteoporosis?
Bone remodelling plays a key role in the development of osteoporosis. However, there are other factors that can increase your risk of developing the disease, such as:

- Sex: Women are at increased your risk of developing osteoporosis due to hormonal changes that arises after menopause.
- Age: The risk of developing osteoporosis increases with age.
- Race: Being Caucasian or Asian has been associated with an increased predisposition to osteoporosis.
- Body frame size: People who have small body frames may have less bone mass to draw from as they age, hence increasing their risk of developing the disease.
- Family history: Having a parent of sibling affected by osteoporosis, increases your risk of having it.
- Sex hormones: The reduction of oestrogen release in post-menopausal women and testosterone in older men, increase their risk of developing osteoporosis. In addition, medications that lower your hormone levels can also contribute to the disease.
- Thyroid disorders: Excessive amount of thyroid hormones either due to thyroid disorders or medications can increase your of developing osteoporosis.
- Parathyroid and adrenal problems are associated with osteoporosis.
- Eating disorders: Being underweight and excessively restricting food intake weakens the bone.
- Low calcium intake: This contributes to reduced bone density, early bone loss and increased vulnerability to fractures.
- Gastrointestinal surgeries: Surgeries that are done for gastrointestinal disorders or weight management often limits the amount of surface area available to absorb nutrients such as calcium. This occurs as a result of reducing the size of the stomach or removing part of the intestines.
- Medications: Long-term use of corticosteroids such as cortisone and prednisone interferes with the bone remodelling process. In addition, drugs that are used in the management of diseases such as gastric reflux, organ transplant rejection, cancer or seizure are associated with osteoporosis.
- Medical conditions: Certain medical conditions are associated with osteoporosis, such as celiac disease, kidney or liver disease, inflammatory bowel disease, lupus, cancer, rheumatoid arthritis or multiple myeloma.
- Cigarette smoking: This contributes to the development of weak bones.
- Alcohol abuse: Excessive alcohol consumption increase your risk of developing osteoporosis.
- Sedentary lifestyle: Regular physical and weight-bearing exercises are beneficial for your bones. People who sit for long hours are at increased risk of developing the disease.

Symptoms of osteoporosis
Early stages of bone loss is often asymptomatic. However, as the disease progresses, your bone becomes weaker and weaker resulting in symptoms such as:
- Neck and back pain: either due to fractures or collapse of your vertebrae.
- A stooped posture
- Loss of height: usually due to a compression fracture in the vertebrae of the neck or back.
- A fragile bone that breaks too easily either as a result of a fall or a strong sneeze or cough.

Making diagnosis
The diagnosis of osteoporosis starts by a thorough history taking so that your doctor understand your symptoms better which is usually followed by a physical examination. Several tests can be performed to assess or diagnose osteoporosis, such as:
- Blood tests:
- Complete Blood Count (CBC): CBC is usually done to rule out anaemia as chronic anaemia predisposes you to bone loss.
- Serum chemistry levels: this is to measure the levels of calcium, phosphate, magnesium and creatinine.
- Liver function test: increased level of alanine aminotransferases (ALT), aspartate aminotransferases (AST), Gamma-glutaryl transferase (GGT), bilirubin and alkaline phosphatase may indicate alcohol abuse.
- Thyroid function test: this test is used to rule out any thyroid dysfunction as it is associated with osteoporosis.
- 25-hydroxy Vitamin D level: low vitamin D level predisposes you to osteoporosis.
- Biochemical markers of bone turnover: this test reflects on bone formation and bone resorption in your body as high bone turnover is associated with osteoporosis.
- Plain radiography: if any fracture is such as compression fraction of the spine is suspected, your doctor may request this test to assess the overall skeletal integrity.
- Dual-Energy X-ray Absorptiometry (DXA): DXA is used to measure your Bone Mineral Density (BMD) which is the best indicator of fracture risk.
- Quantitative Computed Tomography (QCT): QCT measures the spinal BMD and is the most sensitive method for diagnosing osteoporosis. In addition, it is useful to identify fractures.
- Single-Photon Emission Computed Tomography (SPECT): SPECT is a bone imaging technique that offers a better image contrast and provides accurate information about the location of the fracture.
- Quantitative ultrasonography: this test is only warranted to be used on the heels. It is a low-cost test and does not involve any radiations. However, it is not as accurate as the other tests.
- Magnetic Resonance Imaging (MRI): MRI is very useful in identifying fractures. It can differentiate between acute and chronic vertebral fractures.
- Bone scanning: this test uses a radioactive substance known as Technetium-99 that detects abnormal increases in bone resorption.
- Bone biopsy: It is done to mainly rule out conditions like multiple myeloma.

Treatment of osteoporosis
Unfortunately, there is no cure to osteoporosis. However, there are several drugs and lifestyle modifications which can be used to strengthen and protect your bone, including:
- Bisphosphonates: they are used to prevent none loss and is the most common drug used in the management of osteoporosis. Examples include alendronate and ibandronate.
- Hormonal Replacement Therapy (HRT): it is used during and after menopause to stop bone loss.
- Testosterone: In men, this helps to increase bone density.
- Selective estrogen receptor modulator: this drug is used to prevent bone loss and used in postmenopausal women. An example is raloxifene.
- Parathyroid hormone (PTH): PTH helps to prevent bone loss which is used in postmenopausal women with severe osteoporosis. An example is teriparatide.
- Monoclonal antibody: this drug increases bone formation and an example is romosozumab.
- Humanized monoclonal antibody: this drug decreases bone resorption and is used especially in people with renal impairment. An example is denosumab.
- Calcitonin: This is a hormone that decreases bone resorption thereby impeding postmenopausal bone loss. It is used in people who cannot use estrogen therapy. In addition, it has to be taken with calcium and vitamin D supplements.
- Diet: eat foods containing calcium and vitamin D everyday such as fish, dairy products, cheese, egg yolk and beef liver.
- Lifestyle modification: weight-bearing exercises such as climbing stairs, squats and push-ups amongst others will help to trigger bone formation and strengthen your bones. Smoking cessation and reduction of alcohol use may also help.

Complications of osteoporosis
Bone fracture, especially in the hip or spine are the most feared and severe complications of osteoporosis. In addition, the fracture most commonly results from a fall which may even cause disability. Consequently, this increase the risk of death within the first year of the injury. Furthermore, vertebral fractures can even occur without a history of fall. This is because your vertebrae becomes so fragile that it crumples leading to loss of height, stooped posture, neck and back pain.

Prevention of osteoporosis
Good nutrition and regular exercises are fundamental for keeping your bones healthy throughout life. This is why the recommended daily amount of calcium & vitamin D, smoking cessation and weight-bearing exercises are advised for the prevention of osteoporosis.
Prognosis
Prognosis of osteoporosis is good provided that bone loss is detected early and proper management is undertaken. Prevention of falls is of utmost importance in susceptible people. However, fractures in people with osteoporosis are associated with a significantly poorer prognosis.

Source:
J. Alastair, I. and Simon, M., 2016. Davidson’s Essentials of Medicine. 2nd ed. London: ELSEVIER.
Parveen, K. and Michael, C., 2017. Kumar & Clarks Clinical Medicine. 9th ed. The Netherlands: ELSEVIER.
Elam, R., 2020. Osteoporosis
Porter JL, Varacallo M. Osteoporosis. 2020 Jan.
Johnston CB, Dagar M. Osteoporosis in Older Adults. Med Clin North Am. 2020 Sep. 104 (5):873-884.