What is reactive arthritis?
Reactive arthritis, previously known as Reiter syndrome, is an autoimmune disease that develops following an infection. It has been known to follow various infections affecting the gastrointestinal tract (Shigella, Salmonella, Campylobacter, and other pathogens) as well as infections affecting the genitourinary system (Chlamydia trachomatis).
Reactive arthritis usually present with a triad of symptoms, including: arthritis (joint pain), conjunctivitis (eye inflammation) and urethritis (inflammation of the tube carrying urine out of the body-urethra). It is estimated to affect around 3-5 people per 100,000. It may be more common among people who have acquired immunodeficiency syndrome. The disease tends to be more severe and impairing in individuals in lower socioeconomic classes. Reactive arthritis is most common among young men especially those in their thirties. The disease is rare among children.
What are the causes and risk factors of reactive arthritis?
Reactive arthritis is a condition that is triggered by an infection in the genitourinary or gastrointestinal tract. In most cases, you may not even be aware of the triggering infection as there may be minimal or no symptoms at all. There are several bacteria that can cause the disease. These include:
- Chlamydia
- Salmonella
- Shigella
- Yersinia
- Campylobacter
- Clostridium difficile
Reactive arthritis, as it is, is not a disease that can be transmitted. However, the bacteria can be transmitted through sexual intercourse or in contaminated food.

You are at increased risk of having reactive arthritis if you:
- Are aged between 20 and 40
- Are a man
- Have hereditary predisposition to have the disease
What are the signs and symptoms of reactive arthritis?
Reactive arthritis usually begins 2-4 weeks after an infection in the genitourinary and gastrointestinal tract. In some people the infection may not be apparent. The classic triad of symptoms of reactive arthritis occurs in only one third of all patients with the disease. In many people the conjunctivitis and urethritis arises weeks before the person actually seeks medical attention. The symptoms that may be present in reactive arthritis include the following:
- Joint pain mainly in the knees, ankles and feet. In some cases pain may be present in the lower back
- Eye inflammation also known as conjunctivitis
- Painful urination due to urethritis (inflammation of the urethra)
- Malaise
- Fatigue
- Fever
- Muscular pain
- Joint stiffness
- Increased eye tearing
- Increased eye sensitivity to light
- Visual disturbances
- Diarrhoea
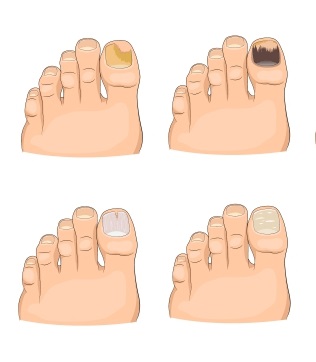
- Skin rash
- Mouth sores

How is the diagnosis of reactive arthritis made?
 To make the diagnosis of reactive arthritis, your doctor will start by asking you a series of questions to know more about your symptoms. Make sure to mention any preceding episodes of infections, eye inflammation and painful urination. He/she will then perform a thorough physical examination to look for signs of reactive arthritis. The diagnosis of reactive arthritis is mostly made based on a good clinical history and physical examination. There are no specific test to make the diagnosis of the condition. However, certain tests may be requested to help in the diagnosis. These include:
To make the diagnosis of reactive arthritis, your doctor will start by asking you a series of questions to know more about your symptoms. Make sure to mention any preceding episodes of infections, eye inflammation and painful urination. He/she will then perform a thorough physical examination to look for signs of reactive arthritis. The diagnosis of reactive arthritis is mostly made based on a good clinical history and physical examination. There are no specific test to make the diagnosis of the condition. However, certain tests may be requested to help in the diagnosis. These include:
- Blood tests: Some markers of inflammation may be found in high levels in the blood in the cases of reactive arthritis. These include: erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP). Anemia may also be found on blood tests. If you are suspected to also have HIV based on your clinical history, tests may be ordered accordingly.
- Urine analysis: In some cases, samples of your urine may be sent for further examination. This includes looking for the presence of white blood cells, red blood cells and proteins in the urine. Some bacteria may also be found in urine analysis.
- Genetic markers: Laboratory tests may also be done to look for specific genetic markers (HLA-B27) which is associated with an increased risk of having reactive arthritis.
- Radiography: X-rays may be requested to look at changes in the joints. However, in some cases of reactive arthritis, there may be no changes in the joints at all despite the presence of joint pain.
- Joint fluid analysis: Arthrocentesis is a procedure in which fluid from joints are collected for further analysis. This must be done to rule out the presence of an infection inside the joint.
How is reactive arthritis managed?
The main goal of treatment for reactive arthritis is to relieve symptoms and treat any coexisting infections. Treatment options include the following:

- Antibiotics: If your doctor finds that your reactive arthritis has been triggered by a bacterial infection, he/she may prescribe you with antibiotics to fight the infection.
- Nonsteroidal anti-inflammatory drugs (NSAIDs): These medications are used to relieve inflammation and the pain associated with reactive arthritis.
- Corticosteroids injection: In some cases, corticosteroids may have to be injected in affected joints to relieve the symptoms of inflammation and pain. This also helps to regain function of your joints for your activities of daily living.
- Steroid creams: These are useful if you have skin rashes associated with reactive arthritis.
- Physical therapy: This is useful for helping with joint and muscle movement. This improves range of motion and joint’s flexibility.
What are the potential complications of reactive arthritis?
The following complications may arise from reactive arthritis:
- Recurrent joint pain
- Chronic joint pain
- Ankylosing spondylitis
- Narrowing of the urethra
- Increased pressure inside the eyes
- Cataracts
What is the prognosis for reactive arthritis?
The course of the disease varies from person to person. However, it most often follows a favourable course where it resolves on its own. Resolution usually occurs within 3-12 months. Death occurs very rarely, and is mostly due to the side effects of the treatment for the disease. In 15-50% of cases, reactive arthritis tend to recur. Reactivation may be due to a newly contracted infection or a stress factor. 15-30% of people end up with long-term and sometimes destructive joint inflammation.


Source:
Lozada, C., 2020. Reactive Arthritis.
Cheeti A, Chakraborty RK, Ramphul K. Reactive Arthritis. 2020 Jan.
Schmitt SK. Reactive Arthritis. Infect Dis Clin North Am. 2017 Mar 11.
Carter JD, Hudson AP. Reactive arthritis: clinical aspects and medical management. Rheum Dis Clin North Am. 2009 Feb. 35(1):21-44.
Pöllänen R, Sillat T, Pajarinen J, Levón J, Kaivosoja E, Konttinen YT. Microbial antigens mediate HLA-B27 diseases via TLRs. J Autoimmun. 2009 May-Jun. 32(3-4):172-7.