What is Anaphylaxis?
Anaphylaxis is a severe form of allergic reaction that usually develops rapidly. If left untreated, it can even result in death. It can be triggered by food, medications or insect bites amongst others. Once your body encounters these allergens, specific cells in your body start to release substances known as chemical mediators leading to the symptoms of anaphylaxis. The mediators travel all around the body affecting various organ systems. The most commonly affected systems include the cutaneous (skin), respiratory, cardiovascular and gastrointestinal system.
Anaphylaxis is unpredictable and can happen anytime. In some cases, it arises in people with known allergies who have been exposed to the allergens, most commonly accidentally, or it can occur for the first time without any prior episode of allergy. Even if it is the first episode, it can be fatal. Anaphylaxis is a medical emergency that requires prompt recognition and treatment.
What causes anaphylaxis?
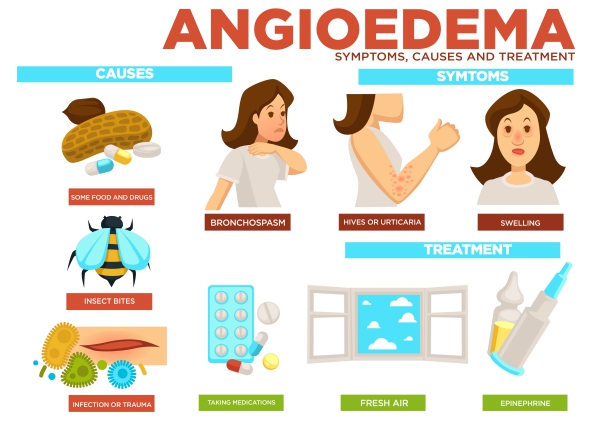
Anaphylaxis occurs due to an allergic reaction in response to certain allergens. When the allergen enters your body through different routes such as oral, respiratory or through the skin, cells in your body produce chemical substances which results in an anaphylactic reaction. Anaphylaxis can be triggered by a variety of allergens. Some of the potential triggers include:
- Food allergens: Anaphylaxis can occur in people consuming eggs, cow’s milk, peanuts, tree nuts, wheat, soy, fish, and crustaceans such as shrimps. In some cases, it can arise following ingestion of certain fruits, vegetables, seeds, spices and food additives.
- Medications: Some antibiotics or painkillers may also result in an anaphylactic reaction in some individuals.
- Insect bites: Venom from certain insects such as bees, wasps, hornets and fire ants can cause an allergic reaction.
- Dyes: Some dyes used for imaging purposes in medicine such as CT scans and other special X-rays can lead to anaphylaxis.
- Latex: Latex gloves, balloons, condoms, sports equipments and medical supplies can also trigger a reaction.

Most people having anaphylaxis already have known allergies to the concerned allergen. These people have already encountered the allergen in the past and have not developed an allergic reaction to it. Instead, the body has produced immunoglobulin E (IgE) which is an antibody. These antibodies stick to specific cells known as mast cells and basophils. When the person is exposed again to that same allergen later, a strong allergic reaction is initiated when the mast cells and basophils come in contact with the allergen. The reaction can be so severe that the condition can become life-threatening.
What are the risk factors for anaphylaxis?
The following factors may make you more prone to have anaphylaxis:
- History of previous severe allergic reactions: If you have had a severe allergic reaction in the past, you are more prone to have same if exposed again to that allergen.
- Medical conditions such as asthma or other chronic lung diseases: These conditions increase your likelihood of having severe respiratory symptoms during an episode of anaphylaxis.
- Other diseases: Heart diseases, for examples, coronary artery disease, make you more prone to have severe anaphylactic attacks.

What are the symptoms of anaphylaxis?
Once you encounter the allergen triggering an anaphylactic attack, the symptoms of anaphylaxis usually arise within minutes to an hour after exposure. Anaphylaxis can lead to symptoms affecting various parts of the body, including:
- Skin: Itchiness, flushing of skin, hives (also known as urticaria) and swelling (also known as angioedema) are the most common symptoms arising in anaphylaxis.
- Eyes: Itchiness, increased lacrimation, reddening of the eye and swelling around the eyes may also occur in anaphylaxis.
- Nose and mouth: Many people experience sneezing, runny nose, congested nose and swelling of the tongue. Some people may also notice a change of taste in the mouth (metallic taste).
- Lungs and throat: These are the most dangerous symptoms that may arise in anaphylaxis. These include difficulty to breathe, repeated coughing, feeling of tightness on the chest, abnormal breath sounds (high pitched sound also known as wheezing), swelling of the throat, change in the voice and choking sensation. When these symptoms arise, prompt treatment should be initiated.
- Heart and circulatory system: Some people may experience dizziness, weakness, loss of consciousness and irregular heartbeats. The blood pressure may also drop in some cases.
- Digestive system: Nausea, vomiting, abdominal pain and diarrhoea may also arise.
- Nervous system: Many people feel anxious, confused and feel like they are almost dying.

How is the diagnosis of anaphylaxis made?
The diagnosis of anaphylaxis should be made as early as possible as it is a medical emergency. In severe reaction, there is no time for tests or laboratory workups. The diagnosis is mostly made based on the clinical history and physical examination. The history will focus on possible exposure to allergens as well as history of previous allergic reactions. In rare cases, laboratory tests may be requested, given that the life of the person is not immediately threatened.
How is anaphylaxis treated?
Once you get the above mentioned symptoms, it is recommended that you seek medical help immediately. If left untreated, many anaphylactic reactions can lead to death.
If you have a known history of allergy, it is advised that you have at your disposition at least one epinephrine autoinjector. It is a device that looks like a pen, containing a medication known as epinephrine. To use the epinephrine autoinjector, you should remove the cap, holding the autoinjector in your fist. Push the end of the pen with the needle firmly against your thigh halfway between your hip and knee. It can be injected on bare skin or through your clothes itself. You should keep holding it for about 3 seconds while all the medication is being injected. You may then remove the needle by pulling it straight out and massage the area where the injection has been made. Epinephrine is the most effective treatment for anaphylactic reactions. Other medications such as antihistamines (which may be effective against hives or itching) or asthma inhalers cannot be used to substitute for epinephrine.

Even after having injected the epinephrine, it is still recommended to head towards the nearest hospital where healthcare professionals will monitor and evaluate your condition and give other treatments if needed. This is important as many anaphylactic reactions occur in two phases: symptoms resolve and recur even if the trigger has been removed.
How can anaphylaxis be prevented?
The most effective way to prevent anaphylaxis is to avoid the triggers. You may seek help from an allergist to do necessary testing in order to know exactly what you are allergic to. If you are allergic to a specific food, it should be completely removed from your diet. If you are eating away from home, ask carefully about the preparation and contents of what you are eating. As a safety measure, always carry your epinephrine autoinjector wherever you go. If you are allergic to an insect bite, avoid places where they are likely to be found or take necessary precautions to avoid stings.
Source:
Mustafa, S., 2018. Anaphylaxis
Kemp SF, Lockey RF. Anaphylaxis: a review of causes and mechanisms. J Allergy Clin Immunol. 2002 Sep. 110(3):341-8.
Simons FE. Anaphylaxis. J Allergy Clin Immunol. 2008 Feb. 121(2 Suppl):S402-7; quiz S420.
Kemp, S., 2020. Pathophysiology of anaphylaxis
Kelso, J., 2020. Anaphylaxis: Confirming the diagnosis and determining the cause(s)
Campbell, R., Kelso, J., 2020. Anaphylaxis: Emergency treatment