What is Appendicitis?
The appendix is a worm-like extension protruding at the beginning of your large intestine. It is found in your lower right abdomen. The function of the appendix is still unknown. When it becomes inflamed, infected or swollen, this condition is called appendicitis. It is a surgical emergency as it can progress to complications such as bursting of the appendix, spreading the infection all around in the abdomen.
The most common cause of the condition is obstruction of the appendix. It is very important to seek medical attention as soon as possible if you suspect having appendicitis as it is a serious condition which can as well be mimicked by other potential life-threatening conditions. It is one of the most common emergencies requiring surgery and cause of pain in the abdomen. In the United States, around 250,000 cases of appendicitis are reported each year. It arises most commonly among teenagers and young adults compared to old people.
The definitive treatment for appendicitis is the removal of the appendix. This procedure is called appendectomy. It may be associated with complications such as infection of the surgical wound.
Causes of Appendicitis
Usually, appendicitis is caused by an obstruction of the lumen of the appendix which is a tube-like structure. Obstruction will result in an increased pressure in the appendix as well as promoting the multiplication of bacteria inside the lumen. White blood cells, which are cells found in the blood fighting against infections, are then recruited in the attempt to resolve the infection. This, however, results in further increase in the pressure inside the appendix due to pus formation and inflammation.

If the increased pressure persist for a long period of time, blood flow in the appendix is compromised resulting in the death of the tissues and increased risk of perforation. It can also result in the formation of an abscess or spread of the infection inside the abdomen.
Obstruction of the lumen of the appendix may be due to several causes including:
- Fecaliths which are stones made of faeces
- Increased amount of tissue present in the appendix, known as hyperplasia
- Parasites such as pinworms
- Foreign bodies
- Tumours
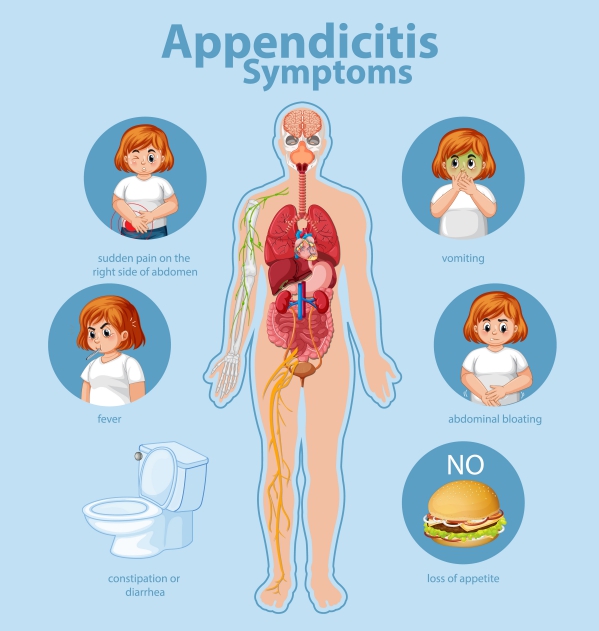
Signs and symptoms of Appendicitis
The appearance of symptoms in appendicitis is usually acute (normally within the last 48 hours). It usually presents with typical symptoms in most individuals. These include:
- Loss of appetite
- Pain around the umbilicus which then moves to the lower right abdomen
- Nausea
- Pain in the lower right side of the abdomen
- Vomiting
- Diarrhoea or constipation
- Fever
If you experience the above symptoms, immediately seek medical help as it can be appendicitis or other serious medical conditions that also need emergent attention.
Making a diagnosis
Your doctor will begin by taking a detailed history from you. This will include questions about your previous surgeries and medical conditions as well as a gynaecological history if you are a female, as the symptoms of appendicitis are similar to those of ectopic pregnancy which is an emergency too. Your doctor will also ask about other symptoms such as painful urination and presence of blood or pus in your urine. These questions are useful to rule out other medical conditions.

Following the history, your doctor will examine you. This will include palpating your abdomen looking for any tenderness or rigid abdomen. A careful physical examination may be enough to make the diagnosis of appendicitis. However, the appendix is not located exactly at the same place in every individual. Because of this variation, further tests may be required to confirm the diagnosis. These tests include:
- Beta –human chorionic gonadotropin (Beta-hCG): It is of utmost importance to perform a pregnancy test in women of childbearing age as an ectopic pregnancy should imperatively be ruled out first. Ectopic pregnancy is when a pregnancy is developing outside the normal location which is the uterus. It most commonly arises in the fallopian tubes. This is a life-threatening condition as the tubes may burst leading to serious complications including death.
- Complete blood cell count: White blood cell count may be increased in the presence of appendicitis as a response to infection and inflammation. However, it is not specific to appendicitis.
- C-reactive protein: This is a substance in the body which increases in response to infection or inflammation. It is very useful in the diagnosis of appendicitis. However, it tends to become normal after 12 hours.
- Urinalysis: Samples of urine may be taken for further examination to rule out conditions of the urinary tract that may present with similar symptoms as appendicitis. The urine is evaluated for the presence of pus, blood or protein.
- Computed tomography (CT) scan: This is an imaging modality that may be used to evaluate for appendicitis. It is usually done with ingestion of a contrast material in people with atypical presentations of appendicitis. The appendix will appear enlarged on the images of the CT scan if appendicitis is present.
- Ultrasonography: Ultrasonography is an imaging technique that uses sound waves to create an image of the structures present in the abdomen. A normal appendix is not usually identified during ultrasonography. However, in the case of appendicitis, whereby the appendix becomes swollen, it can be seen using ultrasound.

Treatment of Appendicitis
The most important thing in the management of appendicitis is to initiate treatment as soon as possible. The earlier management is started, the better the prognosis. There are different steps and treatment options for appendicitis, including:
- Rehydration: Since appendicitis may be associated with vomiting, it is important to replace any fluid loss through intravenous rehydration. You may also be required to not eat or drink anything on your own as you are most likely due for surgery. An antiemetic – medication that suppress vomiting – may also be given to you.
- Painkiller: Appendicitis is most often accompanied by severe abdominal pain. To relieve the pain, painkillers will be administered to you. These may include opioids.
- Antibiotics: Due to the presence of infection in your appendix, antibiotics may also be prescribed in order to fight the bacterial infection. It may also be important to get antibiotics before the surgery in order to decrease the risk of ending up having a wound infection after the surgery.
- Appendectomy: The definitive treatment of appendicitis is the complete removal of the appendix. You can have a completely normal life without your appendix. The surgery can be done in two ways: open or laparoscopic surgery. Open surgery, also known as laparotomy, involves making an incision of about 2-4 inches in your abdomen through which removal of the appendix is done. Laparoscopic surgery is done by making very small incisions through which special surgical instruments and a camera is inserted to perform the surgery. The latter is associated with faster recovery and minimal scarring. The choice between the 2 types of procedures is based on the severity of the condition as well as your general health.
- Abscess drainage: If an abscess is present, a special tube may be used to drain the abscess out through your skin.

Complications of appendicitis
Appendicitis can result in several complications in some cases. These complications include the following:
- Wound infection following surgery
- Perforation of the large intestine
- Intestinal obstruction
- Abscess in the abdomen
- Death
Prognosis
Appendicitis is the most common cause requiring surgery in the abdomen. 4-15% of people having appendicitis will end up with a complication. Therefore, it is very important to make the diagnosis early in order to initiate treatment as soon as possible to improve the outcome. Delay in seeking medical help and in making the diagnosis can significantly impact the course of the disease. Perforation of the appendix is associated with an increased risk of death.


Source:
Craig, S., 2018. Appendicitis.
Martin, R., 2020. Acute appendicitis in adults: Clinical manifestations and differential diagnosis.
Smink, D., 2020. Management of acute appendicitis in adults.