What is cardiac arrhythmia?
Cardiac arrhythmia is a term that groups disorders that result in abnormal heartbeats. It either beats too slowly, too quickly or irregularly. Normally, your hearts rate is of about 60-100 beats per minute. Bradycardia is when the heart beats too slowly, that is, less than 60 beats per minute. If the heart rate is greater than 100 beats per minute, this is called tachycardia.
There are several causes and types of abnormal heartbeats. Some of them are harmless and reversible. However, certain types of cardiac arrhythmias require immediate attention and can be life threatening. They can present with a variety of symptoms and further tests need to be done to confirm which type of arrhythmia is present in order to give the appropriate treatment.
Classification of cardiac arrhythmias
In order to understand the types of cardiac arrhythmias, one should first know how the normal heart usually functions. The heart consists of four chamber. The two upper chambers are the atria and while the two lower chambers are known as the ventricles. The atrium and the ventricle on each side are separated by valves. The way the heart beats is coordinated via a well-defined connection system. It all begins in the sinus node found in the right atrium which acts as a naturally occurring pacemaker. The electrical impulses generated in the sinus node travels through the heart muscle in the atrium and causes its contraction. Blood then flows from the atria to the ventricles. In between the atria and ventricles lies another note called the atrioventricular node. Its function is to relay the electrical impulses to the walls of the ventricles. This results in the contraction of the ventricles and blood is sent all throughout the body and to the lungs.

There are several situations in which your heart may start beating faster and is considered as normal. These include during physical effort or stressful situations. Athletes usually have a slower heart rate as their heart is used to pumping much blood throughout the body.
Abnormalities in the heart rate may originate from different levels of the heart.
Atrial tachyarrhythmias
These types of arrhythmias originate from the atria and causes the heart to beat faster. These include atrial fibrillation, flutter and Wolff-Parkinson-White syndrome.
- Atrial fibrillation: This is a common arrhythmia occurring in 1-2% of the general population and 5-15% of patients over 75 years of age. It can also occur unexpectedly in younger people. This occurs when there is a chaotic and uncoordinated flow of electrical impulses in the atria. Common causes of atrial fibrillation include alcohol intoxication, hyper functioning thyroid, hypertension and heart failure. It can also arise after a cardiac surgery.
- Atrial flutter: This looks a lot like atrial fibrillation. However, the distribution of electrical signals occurs in a more organised fashion.
- Wolff-Parkinson-White syndrome: This involves the presence of an extra electrical pathway between the atria and ventricles resulting in rapid heartbeats.
Ventricular Tachyarrhythmias
In contrast, ventricular tachyarrhythmias originate in the ventricles leading to a rapid heart rate. These include:

- Ventricular tachycardia: In this condition, the ventricles contract so rapidly that they do not have enough time to fill with blood adequately. This results into insufficient amount of blood being expelled from the heart.
- Ventricular fibrillation: This is a serious type of tachyarrhythmia in which there is a completely disturbed flow of signals across the ventricles. The heart is unable to send blood adequately across the body. This requires immediate intervention as it can be fatal.
- Long QT syndrome: This is a condition which can be present from birth or may be acquired later in life. This also results in a fast heartbeat and can even lead to death.
Bradycardia
As mentioned earlier, bradycardia is when your heart rate is less than 60 beats per minute. In certain conditions, it can be due to some pathologies in the heart. There are two ways in which it can happen: either due to the failure of generation of impulse from the sinus node or a problem in the conduction system from the node to the ventricles also known as heart blocks. These include:
- Sick sinus syndrome: This may be due to some pathologic changes in the sinus node impairing its proper functioning. These changes may include scarring. Impulses are slowed down by the sinus node.
- Heart blocks: This can arise following a problem at any level of the conduction system of the heart. There are different degrees of heart blocks varying in severities. In heart blocks, electrical impulses do not travel properly across the wall of the heart.

Risk factors
There are several factors that can increase your risk of having cardiac arrhythmias namely:
- High blood pressure
- Coronary artery disease
- Previous cardiac surgeries
- Inherited cardiac problems
- Disturbed levels of thyroid hormones
- High blood sugar
- Excessive alcohol consumption
- Caffeine
- Cigarette smoking
- Illicit drug use
Signs and symptoms
Cardiac arrhythmias can differ in how they present depending on their type and severity. However, the different types of arrhythmias can have similar signs and symptoms including the following:
- Palpitations (racing heartbeat)
- Slow heartbeat
- Difficulty in breathing
- Fainting or light-headedness
- Pain in the chest
- Irregular pulse
- Decreased blood pressure
- Sweating
- Feeling anxious
Making a diagnosis
If you notice having the above signs and symptoms, it is very important to seek medical advice.
Your doctor will first start by taking a history to know about your existing and past medical conditions as well as for any other clues pointing towards the diagnosis of an arrhythmia.
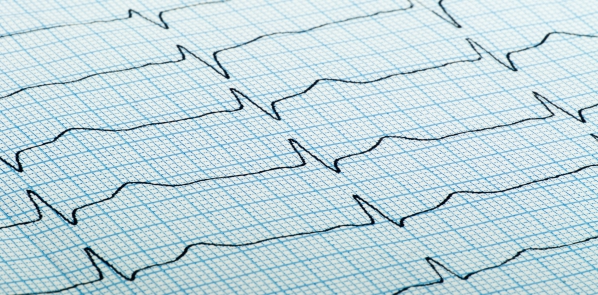
An electrocardiogram (ECG) should be done promptly. This records the electrical activity of the heart and will show if any abnormalities in the conduction of electrical signals is present.

If the ECG does not show any abnormalities there may be the need for further investigations. You may be required to wear a portable ECG which will record your heart rhythm for a 24 hour period. This is known as the Holter monitor.
An echocardiogram may be requested if the above investigations fail to show the abnormalities present. This is a scan of the heart showing the contractions of the atria and ventricles.
Treatment of cardiac arrhythmias
In certain cases, no treatment is required as the arrhythmias may resolve on their own. If the symptoms are too bothersome or the type of arrhythmia is potentially life threatening, treatment may then be needed.
Treatment depends on the underlying cause of the arrhythmia and on whether it causes a fast or a slow heartbeat. Underlying causes should also be treated wherever possible.
Treatments include:
- Medications: These can be used to prevent abnormal heart rhythms or to control the rate at which the heart beats. Blood thinning medications can also be prescribed specifically in atrial fibrillation as there is an increased risk of having blood clots in the heart.
- Cardioversion: In this treatment modality, a special device is used to transmit electric waves to the heart. This gives a shock to the heart causing it to beat back to normal.
- Catheter ablation: A catheter is used to destroy malfunctioning heart tissue that may be causing the abnormal heart rate and rhythm.
- Pacemaker: This is an implantable device that automatically regulates the heart rate acting like the natural pacemaker. It is placed under your skin during a small surgical procedure.
- Implantable cardioverter defibrillator (ICD): This is similar to the pacemaker device in the way that it shocks the heart to make it revert back to its normal rhythm.

Complications
In cardiac arrhythmias, there is an increased risk of blood clotting in your heart. These blood clots can then travel from the heart to other sites of the body such as the brain causing stroke.
Since your heart cannot deliver blood efficiently to the rest of your body, heart failure can occur.
Prevention
Several measures can be implemented to decrease your risk of ending up with a cardiac arrhythmia. These include:
- Smoking cessation
- Decrease or stop caffeine and alcohol consumption
- Stress coping strategies
- Physical activity
- Eating a healthy diet

Source: