What is osteoarthritis?
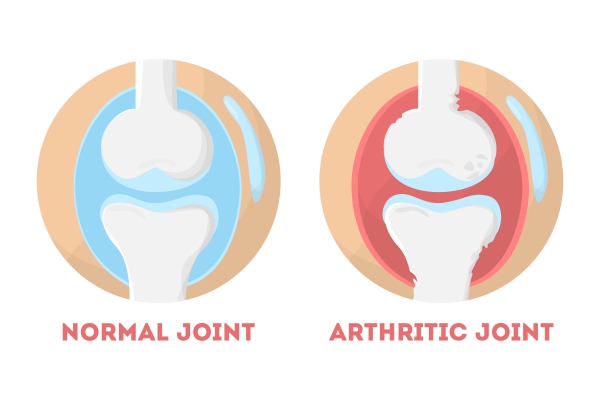
Osteoarthritis is a medical condition affecting many people around the world. This chronic joint disease is actually the most common type of arthritis. The extremities of your bones are covered with a layer of cartilage whose function is to protect your bones during repetitive movements. In osteoarthritis, this protective layer is lost and worn down over time. This leads to friction between two bones causing the appearance of the symptoms.
This disorder can affect any joint in your body but is known to arise most commonly in the joints of your hand, knees, hips and spine. Despite being more commonly seen among the elderly, it can affect any person at any age. This disease can also be called degenerative joint disease due to the degradation of the joint cartilage.
Even if the changes occurring in the joints are irreversible, there exists appropriate treatments to slow its progression and relieve the symptoms.
Causes and risk factors of Osteoarthritis
The main cause of osteoarthritis is the daily stress experienced by the joints. This leads to accumulation of damage to the cartilage. There are several factors that can increase your risk or contribute to the appearance of osteoarthritis namely:
- Increasing age: you are at increased risk of developing osteoarthritis when you are older
- Obesity: being obese puts on more stress on your joints as the latter have to bear more weight causing more wear and tear
- Trauma to the joint: for example, injuries during sports or accidents
- Previous surgery in the joint: this can accelerate the onset of osteoarthritis due to the manipulations inside the joint
- Genetic causes: some people are increased risk of inheriting osteoarthritis
- Previous history of inflammation in the joint
- Bone disorders: this may be associated with weak or malfunctioning cartilage
- Female sex: women are more likely to end up having osteoarthritis compared to man. However, the reason is unknown.
- Certain metabolic disease: such as diabetes or hemochromatosis (a condition in which the body has too much iron)

Signs and symptoms of osteoarthritis
Osteoarthritis is a disease which progresses slowly and gradually start to cause impairment. It occurs more commonly in particular joints such as the hands, knees, hip and spine.
Initially, your joints may appear totally normal, but later, this disorder manifests with a variety of symptoms such as:
- Pain: this symptom is the one which causes the most impairment during your daily activities. The pain may be present during or after any movement of the joint.
- Joint stiffness: this is mostly present when you wake up in the morning or if you have rested for long periods of time
- Decreased range of motion: you may notice that you lose flexibility in your joints
- Tenderness: when pressure is applied on or next to the joint
- Grating sensation: whenever you move your joint you may feel like the structures in your joints are rubbing against each other
- Bone spurs: these can be felt as extra bony prominences around your affected joint
- Swelling: this is secondary to the inflammation going on within your joint

As the disease progresses, the symptoms become more and more severe and impairing. This can be staged according to the symptoms in order to get an idea of the severity. The damages caused by osteoarthritis on the structures present in your joint are irreversible.
Difference between osteoarthritis and rheumatoid arthritis
Even if these two conditions share almost the same array of symptoms, they are very different diseases. Since osteoarthritis is a degenerative disease, its severity will increase with time. In the contrary, rheumatoid arthritis is an autoimmune disorder, which means that it is your own body that is “attacking” your joints to cause disease. This results in painful, inflamed, stiff and swollen joints.
Making a diagnosis
To make a proper diagnosis, it is important to have a clear history, focusing on the appearance of the symptoms and their particularities, followed by some imaging tests and blood tests to rule out any other conditions. The tests are as follows:

- X-rays: even if cartilages are not visible on X-rays, the narrowing of the space between the bones can be visualised. Bony spurs can also be seen on X-rays.
- Magnetic resonance imaging (MRI): this technique is not commonly used but can come handy if a more detailed view is required.
- Blood tests: Osteoarthritis cannot be diagnosed using blood tests. However, it is useful to rule out other diseases that can be causing the same symptoms such as rheumatoid arthritis.
- Joint fluid analysis: some fluid can be aspirated from your affected joint using a needle to be sent for examination. This can tell you whether the symptoms are being caused by gout or an infection rather than osteoarthritis.
Treatment of Osteoarthritis
Management of most medical conditions start with proper lifestyle modifications which can help to change the course of the disease. These include:
- Exercise: It is recommended to get some physical exercise into your schedule. This will help to increase your endurance as well as making your joints stronger and more stable. However, be cautious not to overdo it; start with low intensity exercises and gradually work your way up as far as you feel that you can tolerate it. Some examples of exercises include yoga, tai chi, walking, swimming and cycling.
- Lose weight: If you are overweight, your extra pounds put a lot of work on your weight-bearing joints. Losing these extra pounds will relieve your joints and decrease the amount of damage on your cartilage. Exercise, portion control and healthy eating can help you lose weight.
- Sleeping well: this will help alleviate inflammation and swelling when you are resting.
- Compress: hot or cold compress can be used to relieve pain and stiffness in your joints. These can be applied for about 15 to 20 minutes multiple times daily.

There is no definitive cure for osteoarthritis. The available drugs are useful for symptom relief and slowing down the progression of the disease. The medications most commonly used are:
- Acetaminophen: this can help some people in the management of pain caused by osteoarthritis. However, the recommended dose should not be exceeded as this can cause liver damage.
- Nonsteroidal anti-inflammatory drugs (NSAIDs): for example: Ibuprofen and naproxen sodium. These drugs also relieve the pain caused by the disease. Some side effects may include: stomach upset, bleeding problems, cardiovascular, liver and kidney problems. Topical NSAIDs are also available, for example diclofenac.
- Duloxetine: this medication has shown to be effective in cases with chronic pain.
- Corticosteroid: This drug is available in both oral and injectable form. Usually, it is directly injected into the joint for significant pain reduction.
- Hyaluronic acid: this is also injected inside joints for lubrication. This substance is similar to the fluid naturally found inside your joints.
In some cases, medications and lifestyle modifications are not enough for symptom relief and functional improvement. Surgery may then be the only left treatment. The possible procedures include:

- Osteotomy: this procedure also known as bone realignment, is whereby a surgeon cuts a bone to make it shorter or longer in order to change its alignment in the affected joint. This will shift your body weight in such a way that it relieves pressure from the damaged areas of your joint.
- Arthroplasty: this is when your damaged joint is removed and replaced by metal or plastic structures. These will need to be replaced whenever they are worn out or become loose.
Complications of Osteoarthritis
In the long run, several complications may arise due to osteoarthritis:
- Reduced mobility
- Chondrolysis: loss of bone tissue due to the rapid erosion of cartilage
- Osteonecrosis: death of bone tissue
- Fractures: due to the stress on the bones
- Bleeding in your joints
- Infections in your joints
- Unstable joints
- Sleep disruption: due to pain
- Weight gain: due to decreased activity
- Anxiety and depression
Prevention of Osteoarthritis
Even if there are some factors that are beyond your control, there are certain things that can be done to prevent the occurrence of osteoarthritis:
- Wear appropriate footwear: if you are someone who exercise a lot, an athlete or if you move around a lot, you should wear appropriate footwear or athletic supports that will reduce the impact on your knee joint, hence decreasing the amount of wear and tear on your cartilage.
- Maintain a healthy weight
- Get enough rest

Prognosis of Osteoarthritis
This disease follows a chronic course and does not have a definitive treatment. However, with appropriate management and early recognition of the symptoms, the outlook is positive. It is important to know about the presentation of the disease and seek medical attention accordingly.

Source: