What is Psoriatic Arthritis?
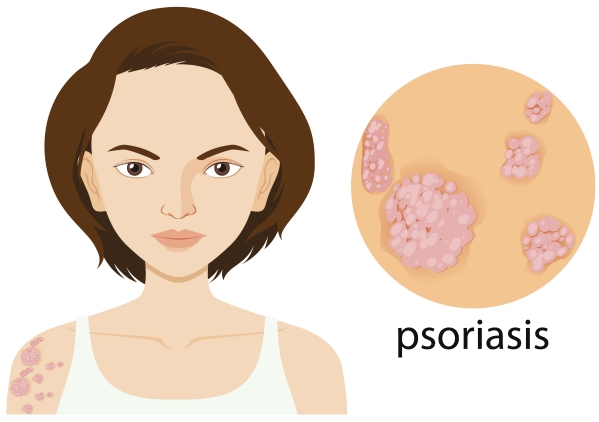
Psoriatic arthritis is an inflammatory condition that affects several joints of the body with coexisting psoriasis. Psoriasis is a skin condition that occurs when the cells found in your skin, called keratinocytes, proliferate too much causing an accumulation of skin cells. This accumulation manifests as white plaques on the skin. It can arise in several areas of the body. Psoriatic arthritis is the most common seronegative (meaning that blood tests are negative) inflammatory joint condition present in people with psoriasis. One of five people having psoriasis also have psoriatic arthritis.
Studies have shown that psoriatic arthritis is more common in people with severe psoriasis compared to those with mild disease. When it arises in people aged above 60 years, the disease tends to have a more severe onset and a more destructive course compared to younger patients. The course of the disease is similar to psoriasis itself, that is, it comes and goes (waxing and waning pattern).
There are several types of psoriatic arthritis including:
- Asymmetrical oligoarticular arthritis: This is the most common type of psoriatic arthritis. It affects the finger and toes at first resulting in a typical “sausage” appearance of the digits. The knee is also commonly involved.
- Symmetrical polyarthritis: Also known as the rheumatoid-like pattern, this affects the hands, wrists, ankles and feet. However, rheumatoid factor is not present on blood tests.
- Distal interphalangeal arthropathy: In this type of psoriatic arthritis, the small joints of the fingers are involved. The nails are also commonly involved.
- Arthritis mutilans: In this rare form of psoriatic arthritis, there is bone destruction with severe finger deformation.
- Juvenile psoriatic arthritis: This type of juvenile psoriatic arthritis, as the name suggests, occurs in children. It accounts for 8-20% of joint inflammation in children.

What are the causes of psoriatic arthritis?
The exact mechanism through which the disease occurs is not well understood. There are several factors that may contribute in the development of the disorder. These include:
- Genetic factors: 40% of people with psoriatic arthritis have close family members with the same condition. There are certain genes that may increase your risk of having the disease.
- Immunologic factors: There are some substances that are released by your immune system that can initiate inflammation.
- Environmental factors: In some cases, viral or bacterial infections can trigger psoriatic arthritis. Trauma can also contribute in the development of the condition.
What are the signs and symptoms of psoriatic arthritis?
In 60-80% of patients, psoriasis is the main symptom that precedes psoriatic arthritis. Psoriasis appears as red skin patches with overlying white silvery scales. However, in some other people, the joint inflammation precedes the psoriatic skin involvement. The signs and symptoms of psoriatic arthritis include the following:

- Joint pain
- Joint stiffness
- Fatigue
- Nail changes: Beau lines, white lines, white dots, haemorrhages, thickening of nails
- Sausage-like fingers
- Joint deformation
- Inflammation of the eyes
How is the diagnosis of psoriatic arthritis made?
To make the diagnosis of psoriatic arthritis, your doctor will start by asking you a series of questions to know more about your symptoms. He/she will then proceed with a thorough physical examination to look for signs of psoriatic arthritis. Your doctor will particularly have to make the difference between psoriatic arthritis and rheumatoid arthritis which are two different entities, yet so alike. The following tests may be requested:
- Erythrocyte sedimentation rate: This is an inflammatory marker present in the blood. It is elevated in around 40% of people with psoriatic arthritis.
- C-Reactive protein: This is also an inflammatory marker that can be elevated in the case of psoriatic arthritis.
- Rheumatoid factor: This is a marker for rheumatoid arthritis. If you have psoriatic arthritis, this is likely to be negative. However, in a small percentage of people, it can be positive.
- Synovial fluid: Some of the fluid present in an inflamed joint can be collected for further analysis. This is likely to show the presence of inflammation in the case of psoriatic arthritis.
- Imaging: Imaging tests can be requested to have a look at the affected joints. This can reveal bone erosion or deformation. The most commonly requested imaging tests are X-rays, computed tomography (CT) scans and magnetic resonance imaging (MRI).

How is psoriatic arthritis managed?
The main goal of treatment is to control the inflammation present in the joints of the body. In most cases, the joint and skin involvement is treated simultaneously. Treatment options include the following:
- Non-steroidal anti-inflammatory drugs: These medications work by relieving pain and reducing inflammation in joints. Some examples include ibuprofen and naproxen sodium. However, if you have kidney, liver or stomach disease, you should avoid the intake of these medications.
- Disease modifying anti-rheumatic drugs: These medications work on the long term as they slow down the progression of the disease. They help in preventing permanent joint damage. Some examples include methotrexate, leflunomide and sulfasalazine.
- Immunosuppressants: These medications work by suppressing the immune system preventing your own body from making more damage to the joints. Some examples include azathioprine and cyclosporine.
- Biologic agents: These medications also keep the immune system under control to prevent further damage to the joint and worsening inflammation. Some examples include: abatacept, adalimumab, certolizumab, etanercept, infliximab and tofacitinib.
- Steroid injections: In some cases, the best management strategy is to inject anti-inflammatory medications directly in the joints.
- Physical therapy: This is particularly important to learn what exercise is good for you as well as to increase joint function and mobility despite the disease.

What is the prognosis of psoriatic arthritis?
Originally, psoriatic arthritis was thought to be mild. However, around 40% of people can develop a type that erodes bones and deform joints. If you have the condition, it is important for you to understand clearly the treatment plan so that you can be able to manage your symptoms and be comfortable with possible self-treatment strategies. Your physical therapist can also provide you with adequate information and exercise plan which works best for you. This is particularly important as the wrong kind of exercise or overexertion can be harmful to you.

Source:
Hammadi, A., 2020. Psoriatic Arthritis.
Ritchlin CT, Colbert RA, Gladman DD. Psoriatic Arthritis. N Engl J Med. 2017 Mar 9. 376 (10):957-970.
Taylor W, Gladman D, Helliwell P, Marchesoni A, Mease P, Mielants H. Classification criteria for psoriatic arthritis: development of new criteria from a large international study. Arthritis Rheum. 2006 Aug. 54(8):2665-73
Reich K, Kruger K, Mossner R, Augustin M. Epidemiology and clinical pattern of psoriatic arthritis in Germany: a prospective interdisciplinary epidemiological study of 1511 patients with plaque-type psoriasis. Br J Dermatol. 2009 May. 160(5):1040-7.
Gladman DD. Psoriatic arthritis. Dermatol Ther. 2009 Jan-Feb. 22(1):40-55.
Häfner R, Michels H. Psoriatic arthritis in children. Curr Opin Rheumatol. 1996 Sep. 8 (5):467-72.