What is Athlete’s foot?
Athlete’s foot, known as Tinea pedis in the medical jargon, is a fungal infection of the soles of the feet and of the spaces between the toes. It is related to the ringworm infection of the body (Tinea corporis), fungal infection of the scalp (Tinea capitis) and jock itch (Tinea cruris). The most common fungi responsible for athlete’s foot is Trichophyton rubrum. The first ever reported case of tinea pedis in the United States was in Birmingham, Alabama in the 1920s.
Athlete’s foot is the world’s most common fungal infection of the skin. At some point in time, around 70% of the world’s population will be infected with tinea pedis. It has no predilection for any ethnic group. It is a condition that can affect both men and women. However, more men are affected compared to women. The incidence of athlete’s foot increases with increasing age with most cases occurring after puberty.
Athlete’s foot usually responds well to antifungal treatments.
What are the causes of Athlete’s foot?
Athlete’s foot is caused by a fungus, most commonly T rubrum. It is the most common cause of tinea pedis worldwide. The fungus invades the superficial layers of the skin and the infection does not usually extend to deeper structures. Sebum, which is a substance secreted by your sebaceous glands in your skin, usually prevents the proliferation of T rubrum. However, the skin of the feet does not contain these glands, hence explaining the likelihood of the infection on the feet and interdigital spaces.

Injuries on the skin of the feet and skin maceration can all contribute to the development of the infection. If you have a weak immune system, you are more likely to have the infection. Damp socks and footwear as well as humid conditions all contribute to the proliferation of the fungus. It is a contagious infection, thus can spread from one person to another through contaminated surfaces such as shoes, floors and towels.
What are the symptoms of Athlete’s foot?
The following symptoms are present in athlete’s foot:
- Itchy and scaly soles
- Scales in spaces between toes
- Painful fissures in between toes
- Lesions with vesicles or ulcers on the feet and interdigital spaces
- Reddened (inflamed) feet and toes

How is the diagnosis of Athlete’s foot made?
To make the diagnosis of athlete’s foot, your doctor will begin by taking a detailed history from you. He/she will then proceed by examining your feet. In some cases, your doctor may have to examine other areas of your body to look for any potential spread.
Most of the time, the diagnosis of Tinea pedis is made simply by looking at it and the clinical history. In some cases, where the diagnosis is doubtful, further tests may be required to confirm the diagnosis. This includes Potassium hydroxide (KOH) test. In this procedure, a sample of the affected skin is scraped off from the foot and is mounted on a microscope slide with KOH solution. This slide is then examined under a microscope to look for the presence of the fungus.

How is Athlete’s foot treated?
The mainstay of treatment for athlete’s foot is medical therapy with the use of antifungals. Antifungal medications are available in the form of creams, ointments, powders or sprays.
Tinea pedis can be managed by the use of topical or oral antifungals or with a combination of both. Topical medications are usually used for around 1-6 weeks depending on the type of medication used. Some examples include luliconazole, naftifine gel or cream, econazole, benzylamines, itraconazole and clotrimazole.
What are the complications of Athlete’s foot?
Athlete’s foot does not usually result in severe complications. However, it can spread to other parts of the body, including:
- The hands: If you are constantly touching or scratching your infected feet, you are likely to have the same infection on your hands.
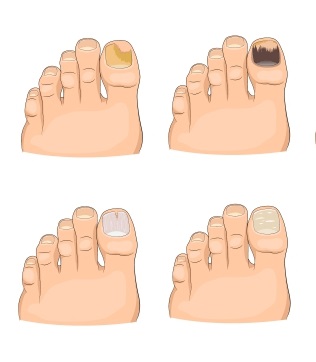
- The nails: If your toenails are affected by the fungus, it becomes more difficult to treat.
- The groin: This condition is known as jock itch. It is when the fungal infection spreads to the groin area most commonly through your hands or using the same towel for the feet and groin area.
How can Athlete’s foot be prevented?
Athlete’s foot can be prevented through the following measures:
- Dispose your old shoes once you have been treated to prevent reinfection. Your shoes may also be treated using antifungal powders.
- Use protective footwear at public pools and baths
- Keep your feet dry by avoiding the use of occlusive footwear
- If occlusive footwear is worn, wear cotton socks and use drying powders with antifungal action in the shoes.
- Wear aerated or open shoes.

What is the prognosis for Athlete’s foot?
Athlete’s foot is a condition whose prognosis depend on the type of infection as well as underlying conditions that coexist such as a weakened immune system and diabetes. With appropriate treatment, the prognosis of tinea pedis is generally excellent. In many cases, the disease may recur if exposed again to the fungus. Old shoes are sources of reinfection and should be disposed or treated with antifungal powders.

Source:
Robbins, C., 2020. Tinea Pedis
Nigam PK, Saleh D. Tinea Pedis. StatPearls [Internet]. 2020 Jan.
Kutlubay Z, Yardımcı G, Kantarcıoğlu AS, Serdaroğlu S. Acral manifestations of fungal infections. Clin Dermatol. 2017 Jan - Feb. 35 (1):28-39.
Gentles JC, Evans EG. Foot infections in swimming baths. Br Med J. 1973 Aug 4. 3(5874):260-2.